Edema refers to abnormal accumulation of fluid in the body’s tissues, leading to visible or palpable swelling. It most commonly affects the legs, ankles, and feet, but can also involve the lungs, abdomen, face, or arms depending on the underlying cause.
Edema is not a disease by itself. Rather, it is a sign of an underlying problem related to fluid balance, blood vessels, the heart, kidneys, liver, or lymphatic system. Understanding why edema occurs is essential for effective treatment.
How Edema Develops
Under normal conditions, fluid moves in and out of blood vessels in a tightly regulated manner. Edema develops when this balance is disrupted, allowing excess fluid to leak into surrounding tissues or when the body is unable to remove fluid efficiently.
Key mechanisms include increased pressure in blood vessels, reduced protein levels in the blood, increased vessel permeability due to inflammation, or impaired lymphatic drainage.
Common Types of Edema
Peripheral Edema
Peripheral edema affects the legs, ankles, and feet and is the most common form. It often worsens after prolonged standing or sitting and may improve with leg elevation.
Pulmonary Edema
Pulmonary edema refers to fluid accumulation in the lungs. It interferes with oxygen exchange and causes shortness of breath. This form of edema is often related to heart disease and is a medical emergency when severe.
Lymphedema
Lymphedema results from impaired lymphatic drainage, leading to persistent swelling—most commonly in the arms or legs. It may occur after surgery, radiation therapy, infection, or due to congenital lymphatic disorders.
Localized Edema
Localized swelling may occur due to injury, inflammation, infection, or allergic reactions and is typically confined to a specific area.
Causes of Edema
Edema can arise from many different conditions. Identifying the cause guides treatment.
Heart-Related Causes
Heart failure is one of the most important causes of edema. When the heart cannot pump effectively, blood backs up in veins, increasing pressure and causing fluid to leak into tissues—especially the legs and lungs.
Kidney Disease
The kidneys regulate salt and water balance. When kidney function is impaired, excess fluid and sodium may accumulate, leading to widespread swelling.
Liver Disease
Advanced liver disease can reduce the production of proteins that help keep fluid inside blood vessels. This can result in leg swelling and fluid accumulation in the abdomen.
Venous Insufficiency
Weak or damaged leg veins can cause blood to pool in the lower extremities, leading to chronic swelling that often worsens throughout the day.
Lymphatic System Disorders
Damage or blockage of lymphatic vessels prevents proper fluid drainage, resulting in lymphedema.
Medications
Certain medications can cause or worsen edema. These include some blood pressure medications, anti-inflammatory drugs, hormones, and medications used to treat diabetes.
Inflammation, Infection, and Injury
Local tissue inflammation increases vessel permeability, allowing fluid to escape into tissues. This type of edema is often painful and associated with redness or warmth.
Symptoms of Edema
Symptoms depend on location and severity.
Common features include:
- Visible swelling or puffiness
- Tight or shiny skin
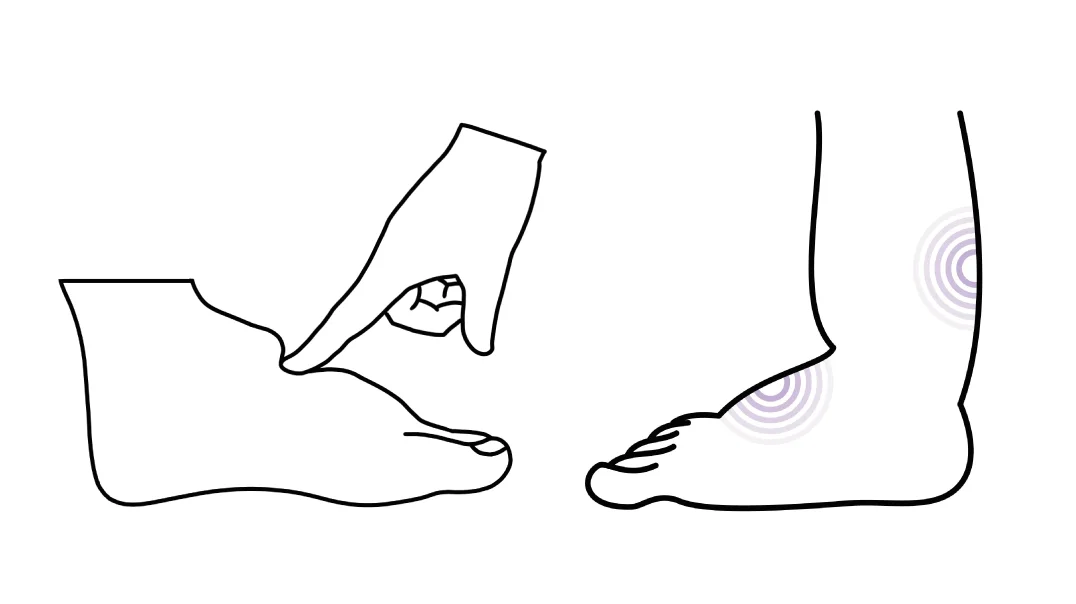
- Indentation after pressing on the skin (pitting edema)
- Heaviness or discomfort in the affected area
- Shortness of breath in pulmonary edema
Sudden or rapidly worsening edema should always be evaluated.
How Edema Is Diagnosed
Diagnosis begins with physical examination and medical history. The pattern and location of swelling provide important clues.
Additional tests may include blood tests, urine studies, heart imaging, ultrasound of veins, chest imaging, or other studies to identify the underlying cause.
Treatment Options for Edema
Treatment focuses on addressing the underlying cause, not just reducing swelling.
Lifestyle and Supportive Measures
For mild peripheral edema, simple measures may be effective. These include leg elevation, avoiding prolonged standing or sitting, regular movement, and use of compression stockings in appropriate cases.
Reducing excess salt intake can help limit fluid retention.
Medications
When edema is related to fluid overload, diuretic medications may be prescribed to help the body eliminate excess fluid. These medications must be used carefully and under medical supervision.
Medication adjustments may be needed if edema is drug-related.
Treating the Underlying Condition
Effective long-term management depends on controlling the condition causing edema, such as heart failure, kidney disease, liver disease, or venous insufficiency.
In lymphedema, specialized therapies including compression, manual lymph drainage, and physical therapy play a central role.
Emergency Treatment
Pulmonary edema or sudden, severe swelling associated with breathing difficulty requires urgent medical care. Treatment focuses on stabilizing breathing and circulation while addressing the cause.
Simple Strategies to Reduce Edema
In addition to treating the underlying cause, several simple measures can help reduce swelling and improve comfort—particularly in mild or chronic peripheral edema.
Leg elevation is one of the most effective strategies. Raising the legs above heart level when resting helps fluid return to the circulation and reduces pooling in the lower extremities.
Regular movement is important. Avoiding prolonged sitting or standing and taking short walks encourages blood and fluid flow, especially in the legs.
Compression stockings, when recommended by a healthcare professional, can support venous return and reduce daily swelling. They are particularly helpful in venous insufficiency.
Reducing salt intake may help limit fluid retention in people prone to edema, especially when swelling is related to heart, kidney, or liver conditions.
Maintaining adequate hydration is also important. Paradoxically, dehydration can worsen fluid retention by triggering hormonal responses that conserve water.
These strategies can improve symptoms but do not replace medical evaluation or treatment. Persistent or worsening edema should always be assessed to identify and manage the underlying cause.
When to Seek Medical Attention
Medical evaluation is recommended for new, persistent, or worsening swelling—especially if it is accompanied by shortness of breath, chest pain, skin redness, or pain.
In Summary
Edema is swelling caused by excess fluid accumulation in body tissues and is a sign of an underlying medical condition rather than a diagnosis itself. Causes range from heart, kidney, and liver disease to venous and lymphatic disorders. Treatment depends on identifying and addressing the root cause while relieving symptoms and preventing complications.
Reference: Edema