Heart failure is a condition in which the heart muscle is unable to pump or fill with blood effectively enough to meet the body’s needs. This may occur because the heart muscle becomes weakened and cannot contract forcefully, or because it becomes stiff and cannot relax and fill properly between beats. In both cases, the result is reduced blood flow to the body and fluid buildup in the lungs or other tissues.
Heart failure is a common and serious condition, but with modern treatment, many people are able to live longer and more active lives. Understanding how heart failure affects the heart muscle—and why it develops—is essential for effective long-term management.
How Heart Failure Affects the Body
The heart’s primary role is to deliver oxygen-rich blood to organs and tissues. When the heart cannot pump effectively, the body compensates by activating hormonal and nervous system responses. While helpful in the short term, these compensatory mechanisms can worsen heart failure over time.
As pumping efficiency declines, fluid may accumulate in the lungs, legs, abdomen, or other tissues. This fluid buildup is responsible for many of the symptoms people experience.
Common Symptoms of Heart Failure
Symptoms of heart failure often develop gradually but may worsen suddenly during exacerbations.
Common symptoms include:
- Shortness of breath, especially with exertion or when lying flat
- Fatigue and reduced exercise tolerance
- Swelling of the legs, ankles, or feet
- Rapid weight gain due to fluid retention
- Persistent cough or wheezing
- Abdominal bloating or loss of appetite
Symptoms may fluctuate and often worsen when fluid balance is not well controlled.
Types of Heart Failure
Heart failure is classified based on how the heart’s pumping function is affected.
- Heart failure with reduced ejection fraction (HFrEF) occurs when the heart muscle is weakened and cannot contract effectively.
- Heart failure with preserved ejection fraction (HFpEF) occurs when the heart muscle becomes stiff and cannot fill properly, even though pumping strength appears normal.
These forms differ in treatment strategies, but both can cause significant symptoms.
Why Heart Failure Develops
Heart failure usually results from conditions that damage or overload the heart over time. Common causes include coronary artery disease, prior heart attacks, long-standing high blood pressure, and cardiomyopathies.
Other contributors include heart valve disease, arrhythmias such as atrial fibrillation, infections affecting the heart, and certain inherited conditions.
Identifying the underlying cause is critical, as treating it can slow progression and improve outcomes.
Heart Failure and Heart Rhythm Disorders
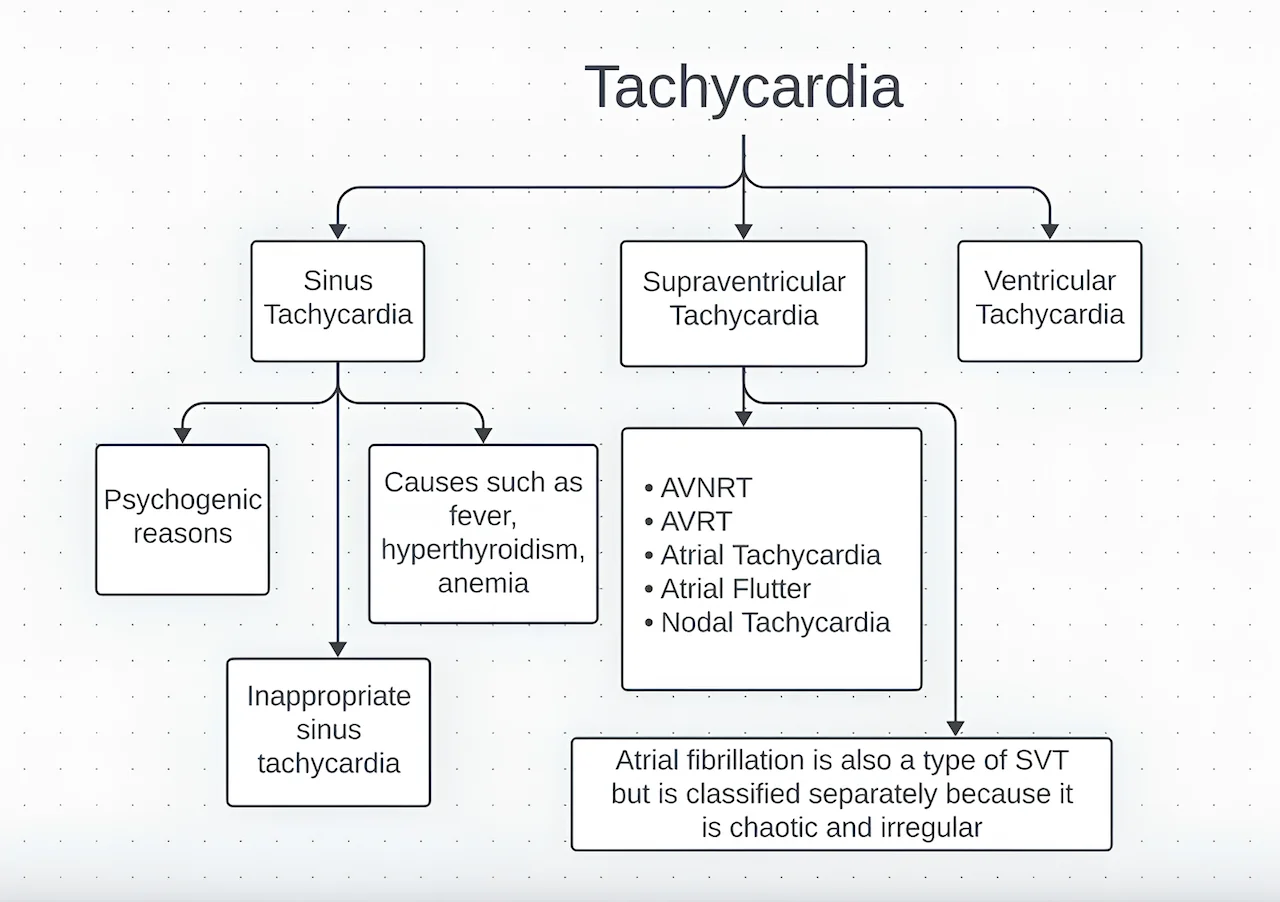
Heart failure and arrhythmias frequently coexist. Structural changes and scarring in the heart increase the risk of rhythm disturbances, while arrhythmias can worsen heart failure by reducing pumping efficiency.
Conditions such as Atrial Fibrillation and ventricular arrhythmias are common in people with heart failure and often require coordinated management.
How Heart Failure Is Diagnosed
Diagnosis of heart failure involves a combination of clinical evaluation, imaging studies, and laboratory testing. The process is aimed not only at confirming the diagnosis, but also at identifying the cause, determining severity, and guiding treatment.
Echocardiography is a key diagnostic test. It provides detailed information about heart size, pumping function (ejection fraction), wall motion, and valve performance. This test helps distinguish between different types of heart failure and plays a central role in treatment decisions.
Blood tests are used to assess organ function and detect contributing conditions. Certain blood markers can help support the diagnosis of heart failure, evaluate its severity, and monitor response to treatment. Tests may also identify anemia, kidney dysfunction, thyroid disease, or electrolyte abnormalities that can worsen symptoms.
Electrocardiography records the heart’s electrical activity and may reveal rhythm disturbances, prior heart damage, or conduction abnormalities that contribute to heart failure.
In selected patients, advanced cardiac imaging is used to further clarify the underlying cause and guide management. Cardiac magnetic resonance imaging (MRI) can identify scar tissue, inflammation, or specific heart muscle diseases. Nuclear imaging or cardiac CT may be performed to assess blood flow to the heart muscle or evaluate coronary artery disease.
Together, these tests provide a comprehensive picture of heart function, allowing treatment to be tailored to the individual patient and adjusted over time.
Treatment Options for Heart Failure
Treatment of heart failure focuses on relieving symptoms, improving quality of life, reducing hospitalizations, and slowing disease progression. Management is almost always multimodal, meaning lifestyle changes, medications, and—in selected cases—device or advanced therapies are combined based on the individual patient.
Lifestyle and Self-Care Measures
Lifestyle measures are not optional in heart failure; they are a core part of treatment.
Reducing salt intake helps prevent fluid retention and shortness of breath. Careful fluid management may be recommended, particularly in patients with recurrent congestion. Regular, moderate physical activity improves exercise capacity and overall cardiovascular health, while excessive exertion should be avoided during unstable periods.
Daily weight monitoring is especially important. A sudden increase in weight often reflects fluid accumulation and may be an early warning sign of worsening heart failure, allowing treatment adjustments before severe symptoms develop.
Medication Therapy
Medications form the cornerstone of heart failure treatment and are tailored to the type and severity of the condition.
Different medications work together to:
- Reduce strain on the heart
- Improve pumping efficiency
- Prevent harmful hormonal activation
- Decrease fluid overload
- Lower the risk of hospitalization and death
Most patients require more than one medication, and doses are carefully adjusted over time. Medication adherence is critical, as stopping or skipping drugs can lead to rapid deterioration.
Device-Based Therapies
In selected patients, devices are used to support heart function and reduce the risk of sudden cardiac events.
Some patients benefit from a specialized form of pacing known as Cardiac Resynchronization Therapy (CRT). CRT is designed for people whose heart chambers do not contract in a coordinated manner due to delayed or abnormal electrical activation.
By pacing both ventricles simultaneously, CRT improves the timing and efficiency of heart contractions. In appropriately selected patients, this therapy can significantly reduce symptoms, improve heart function, decrease hospitalizations, and enhance quality of life.
For patients at increased risk of life-threatening ventricular arrhythmias, an implantable cardioverter-defibrillator (ICD) may be recommended. These devices continuously monitor heart rhythm and can deliver life-saving therapy if a dangerous arrhythmia occurs.
Device therapy does not replace medications but works in addition to optimal medical treatment.
Advanced and Specialized Therapies
When heart failure remains severe despite optimal medical and device therapy, advanced options may be considered.
These include specialized intravenous medications, mechanical circulatory support devices, or referral for heart transplantation evaluation in highly selected patients. Such therapies are typically managed in experienced centers and reserved for advanced stages of disease.
Early referral and timely evaluation are important, as advanced therapies are most effective when initiated before irreversible organ damage occurs.
Living With Heart Failure
Living with heart failure requires ongoing partnership between patients and healthcare providers. Education, adherence to treatment, and early recognition of symptom changes are vital.
Many people with heart failure are able to maintain active lives by following individualized treatment plans and attending regular follow-up visits.
In Summary
Heart failure is a condition in which the heart cannot pump blood effectively enough to meet the body’s needs. It is a chronic condition, but modern therapies allow many patients to manage symptoms, reduce hospitalizations, and improve survival. Early diagnosis, targeted treatment, and active self-care are key to living well with heart failure.
Reference: Heart Failure