Essential hypertension—also known as primary hypertension—is a condition in which blood pressure is persistently elevated without a single identifiable medical cause. It accounts for about 90–95% of all cases of high blood pressure, making it one of the most common chronic health conditions worldwide.
Unlike secondary hypertension, which is caused by an underlying disease, essential hypertension develops gradually over time and is influenced by a combination of genetic, lifestyle, and environmental factors.
- What Is Considered High Blood Pressure?
- How Essential Hypertension Affects the Body
- Causes of Essential Hypertension
- Symptoms of Essential Hypertension
- How Essential Hypertension Is Diagnosed
- Treatment Options for Essential Hypertension
- Long-Term Management and Follow-Up
- Complications of Untreated Essential Hypertension
- In Summary
What Is Considered High Blood Pressure?
Blood pressure is generally considered elevated when systolic pressure is 140 mmHg or higher and/or diastolic pressure is 90 mmHg or higher on repeated measurements.
Essential hypertension is diagnosed when these elevated values persist over time and no specific secondary cause is identified.
How Essential Hypertension Affects the Body
Chronic high blood pressure places continuous stress on the arterial walls. Over time, this leads to vascular stiffening and damage, forcing the heart to work harder to pump blood.
If left untreated, essential hypertension can silently damage vital organs, including the heart, brain, kidneys, and eyes. Because it often causes no symptoms, it is sometimes called the “silent killer.”
Causes of Essential Hypertension
Essential hypertension does not have a single cause. Instead, it develops through the interaction of multiple factors that gradually raise blood pressure over years.
Genetic predisposition plays a major role. Individuals with a family history of hypertension are more likely to develop the condition, particularly when combined with lifestyle risk factors.
Lifestyle and environmental factors are key contributors. High salt intake, excess body weight, physical inactivity, chronic stress, excessive alcohol consumption, and poor sleep quality all promote long-term elevation of blood pressure.
Age-related changes in blood vessels also contribute. As arteries naturally lose elasticity with age, resistance to blood flow increases, raising blood pressure.
In many individuals, essential hypertension represents the cumulative effect of these influences rather than a single trigger.
Symptoms of Essential Hypertension
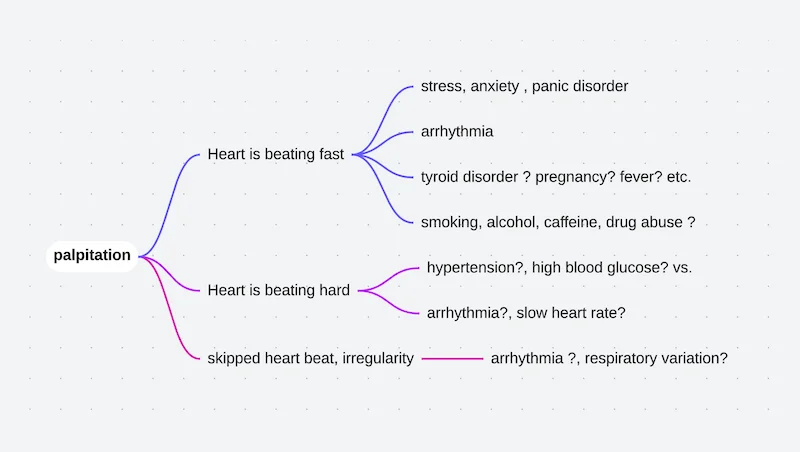
Most people with essential hypertension feel completely well. When symptoms occur, they are often nonspecific and may include headaches, dizziness, shortness of breath, or fatigue.
Because symptoms are unreliable, regular blood pressure measurement is the only way to detect essential hypertension early and prevent complications.
How Essential Hypertension Is Diagnosed
Diagnosis is based on repeated blood pressure measurements taken on different occasions. A single elevated reading is not sufficient.
Home blood pressure monitoring or ambulatory blood pressure monitoring may be used to confirm the diagnosis and rule out temporary or stress-related elevations.
Once hypertension is confirmed, evaluation focuses on assessing cardiovascular risk and identifying any signs of organ damage rather than searching for a specific cause.
Treatment Options for Essential Hypertension
Treatment aims to lower blood pressure safely, reduce long-term cardiovascular risk, and protect target organs. Management is usually lifelong and often combines lifestyle modification with medication.
Lifestyle Modifications
Lifestyle changes form the foundation of treatment and are recommended for all patients, whether or not medications are required.
Reducing salt intake, maintaining a healthy body weight, engaging in regular physical activity, limiting alcohol consumption, managing stress, and ensuring adequate sleep can significantly lower blood pressure. These changes also enhance the effectiveness of medications when they are needed.
Medication Therapy
When lifestyle measures alone are insufficient, antihypertensive medications are prescribed. These drugs work through different mechanisms to lower blood pressure and reduce strain on the heart and blood vessels.
Treatment is individualized, and many patients require more than one medication to achieve optimal control. The goal is consistent blood pressure reduction rather than rapid normalization.
Medication adherence is critical, as untreated or poorly controlled hypertension significantly increases the risk of heart attack, stroke, kidney disease, and heart failure.
Long-Term Management and Follow-Up
Essential hypertension requires ongoing monitoring. Regular follow-up allows adjustment of therapy, assessment of treatment response, and early detection of complications.
Blood pressure targets may be individualized based on age, overall health, and associated medical conditions.
Complications of Untreated Essential Hypertension
If not adequately controlled, essential hypertension increases the risk of:
- Coronary artery disease
- Stroke and transient ischemic attack
- Heart failure
- Kidney disease
- Vision loss
These complications often develop silently over years, reinforcing the importance of early diagnosis and sustained treatment.
In Summary
Essential hypertension is the most common form of high blood pressure and develops gradually due to genetic and lifestyle factors rather than a single identifiable cause. Although often asymptomatic, it carries significant long-term risks if left untreated. With regular monitoring, lifestyle modification, and appropriate medication, essential hypertension can be effectively controlled and its complications largely prevented.
Reference: Primary Hypertension