Heart palpitations are the sensation of being aware of your heartbeat. People often describe them as a fluttering, pounding, racing, skipping, or thumping feeling in the chest, throat, or neck. Although palpitations can be unsettling, they are extremely common and, in many cases, harmless.
What makes palpitations challenging is that the feeling can be intense even when the underlying cause is benign. At the same time, mild or occasional palpitations can sometimes be linked to an underlying heart rhythm problem. This is why understanding what palpitations mean—and when they matter—is so important.
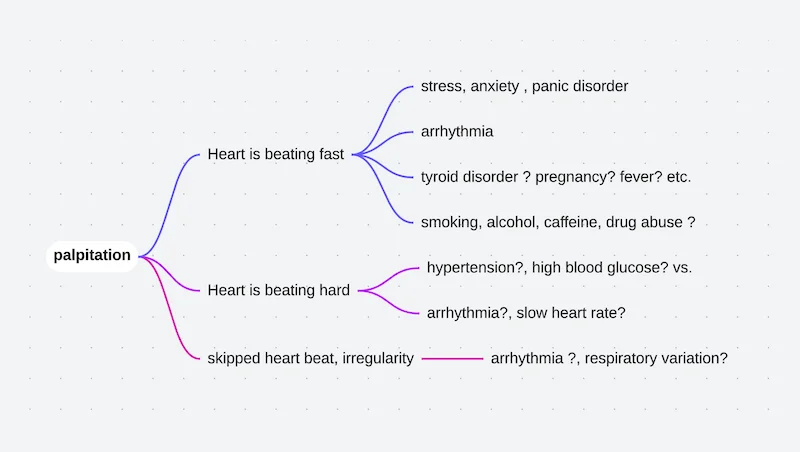
What Do Palpitations Feel Like?
Palpitations do not feel the same for everyone. Some people notice a brief flutter that lasts only a second, while others feel prolonged episodes of rapid or forceful beating.
Common descriptions include:
- A racing heartbeat
- A fluttering or vibrating sensation
- A skipped beat followed by a strong thump
- A pounding sensation in the chest or neck
- Irregular or uneven beats
These sensations may occur at rest, during activity, or when lying quietly in bed, especially at night.
Why Palpitations Are Often Felt So Strongly
In many cases, the sensation of palpitations is not caused by how fast the heart beats, but by how noticeable each beat becomes.
Early or extra beats—such as Premature Atrial Contractions or Premature Ventricular Contractions—are often followed by a slightly stronger heartbeat. This stronger beat is what people usually feel, even though the rhythm disturbance itself is brief.
Increased sensitivity to normal heartbeats, especially during stress or anxiety, can also make palpitations more noticeable without any abnormal rhythm being present.
Common Causes of Heart Palpitations
Palpitations are a symptom, not a diagnosis. They can arise from many different causes, ranging from everyday triggers to true heart rhythm disorders.
Benign and Common Triggers
Many palpitations are related to factors that temporarily stimulate the heart:
- Stress or anxiety
- Caffeine, energy drinks, or nicotine
- Alcohol
- Poor sleep or fatigue
- Dehydration
- Fever or illness
Hormonal changes, including pregnancy or menopause, can also increase awareness of the heartbeat.
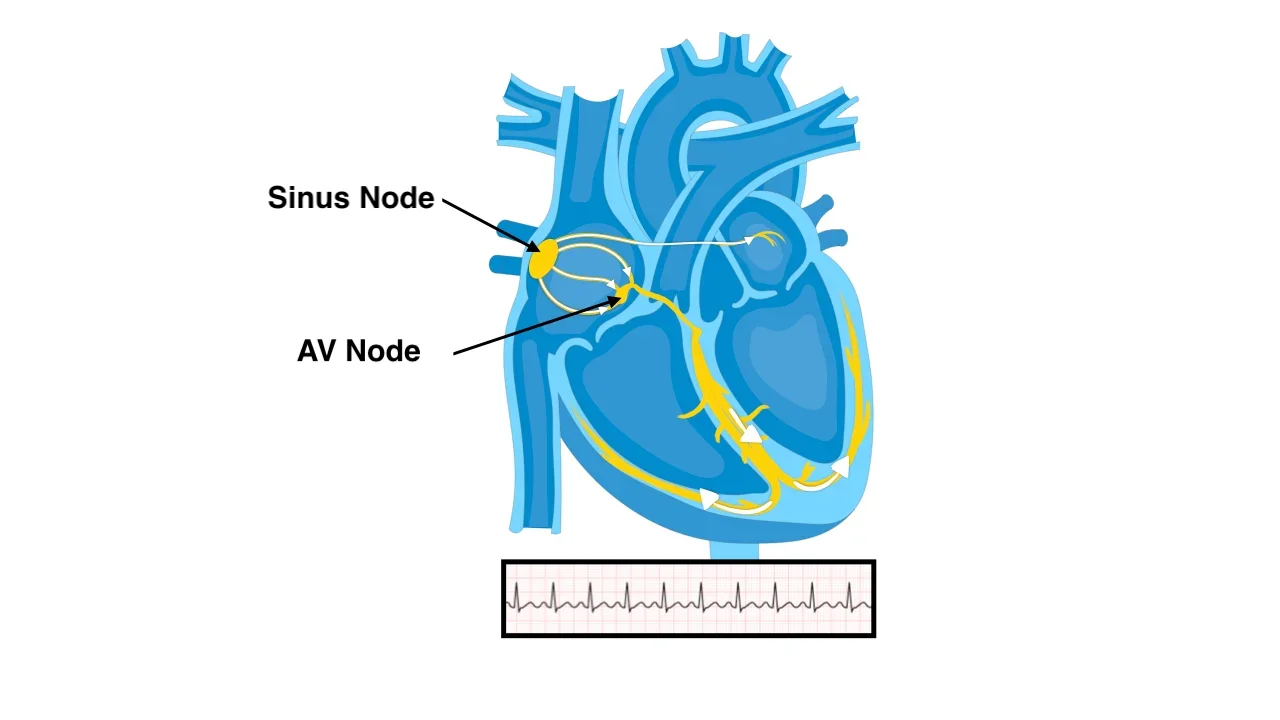
Palpitations Caused by Heart Rhythm Disorders
In some cases, palpitations are caused by a true heart rhythm disorder rather than heightened heartbeat awareness. These arrhythmias may originate in the upper or lower chambers of the heart and differ significantly in both risk and management.
Common rhythm-related causes include Supraventricular Tachycardia, which often begins and ends suddenly, and Atrial Fibrillation, which causes an irregular and often persistent heartbeat. Both conditions commonly produce palpitations and may require targeted treatment.
Palpitations can also originate from the ventricles. Premature Ventricular Contractions are a frequent cause and are often felt as strong thumps or skipped beats. In most people, they are benign, but when very frequent or associated with underlying heart disease, further evaluation is required.
Less commonly, palpitations may be caused by Ventricular Tachycardia, a fast rhythm arising from the lower chambers of the heart. Ventricular arrhythmias are taken more seriously because they can interfere with the heart’s ability to pump blood effectively and may cause dizziness, fainting, or collapse.
Distinguishing between benign ventricular extra beats and more serious ventricular arrhythmias is a critical part of palpitations evaluation.
Palpitations Related to Structural Heart Disease
Not all palpitations are caused by primary rhythm disorders. In some individuals, underlying structural heart conditions can alter the way the heart fills or pumps, leading to increased awareness of the heartbeat.
Conditions such as weakened heart muscle, heart valve disease, or enlargement of the heart chambers may cause the heart to beat more forcefully or irregularly. Even when the rhythm itself is technically normal, these changes can make each heartbeat more noticeable and uncomfortable.
In patients with known structural heart disease, palpitations deserve closer attention, as they may reflect increased stress on the heart or the development of secondary rhythm disturbances. Evaluation in this setting focuses not only on identifying arrhythmias but also on assessing heart structure and function.
When Palpitations Are Concerning
Most palpitations are not dangerous. However, certain features suggest the need for medical evaluation.
Palpitations deserve closer attention when they:
- Occur together with dizziness or fainting
- Are associated with chest pain or shortness of breath
- Happen during physical exertion
- Are very frequent or progressively worsening
- Occur in people with known heart disease
These features raise the likelihood of a significant underlying cause.
How Palpitations Are Evaluated
Evaluation begins with a detailed description of the symptoms. When palpitations start, how long they last, and what triggers or relieves them provide valuable clues.
An electrocardiogram is often performed, but because palpitations may not occur during a brief test, longer-term rhythm monitoring is frequently needed. This helps correlate symptoms with the actual heart rhythm.
Additional tests may be used to assess heart structure, blood tests to identify metabolic causes, or exercise testing when symptoms occur with activity.
Treatment Options for Heart Palpitations
Treatment of heart palpitations depends entirely on the underlying cause. The goal is not simply to suppress the sensation, but to address the mechanism responsible for it while ensuring patient safety and quality of life.
Reassurance and Lifestyle Measures
For many people, palpitations are benign and do not require medical treatment. Once serious causes are excluded, reassurance alone can significantly reduce symptom burden.
Lifestyle adjustments often play a central role. Reducing caffeine, energy drinks, nicotine, and alcohol can markedly decrease palpitations. Adequate hydration, regular sleep, stress management, and avoiding excessive fatigue are equally important. In some individuals, correcting anemia, thyroid imbalance, or electrolyte disturbances completely resolves symptoms.
Medications
When palpitations are frequent or disruptive, medications may be used to reduce their occurrence or intensity. Drugs that slow the heart rate or stabilize electrical activity can help control symptoms, particularly in supraventricular arrhythmias.
Medications are chosen carefully based on the type of rhythm disturbance, underlying heart function, and individual tolerance. The aim is symptom relief and rhythm stabilization rather than eliminating every abnormal beat.
Procedural Treatments
In certain rhythm disorders, procedures can offer long-term or definitive solutions.
Cardioversion may be used when palpitations are caused by sustained arrhythmias such as atrial fibrillation or atrial flutter. This controlled procedure restores a normal rhythm and may significantly improve symptoms.
Catheter ablation is an important option for palpitations caused by specific electrical pathways or focal triggers. By targeting and eliminating the source of the abnormal rhythm, ablation can reduce or completely eliminate palpitations in conditions such as supraventricular tachycardia or frequent premature beats.
In selected patients with ventricular arrhythmias, ablation may also reduce arrhythmia burden and improve symptoms, often as part of a broader treatment strategy.
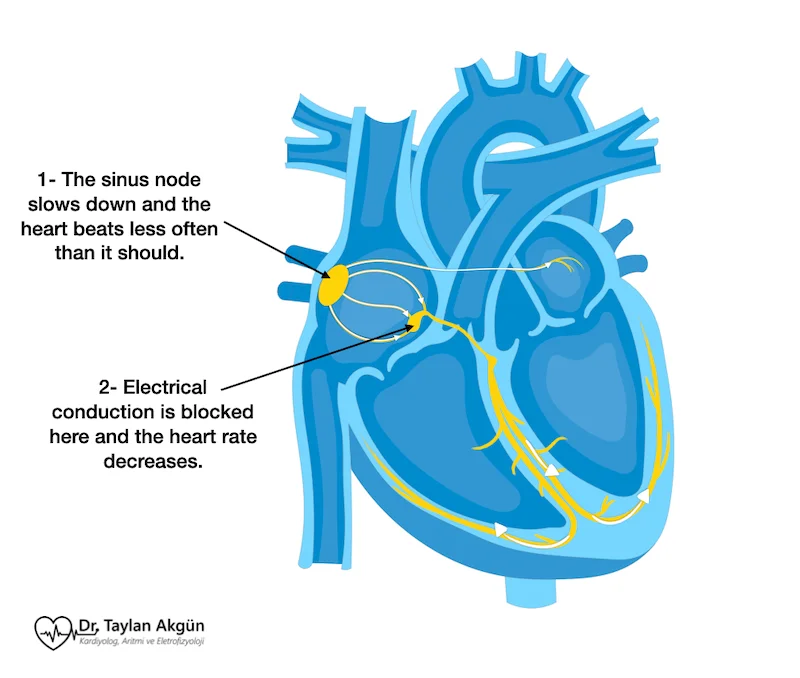
Device-Based Therapy
When palpitations are associated with dangerous rhythms or significant conduction problems, implantable devices may be recommended.
A Pacemaker may be used when palpitations are related to slow heart rhythms or pauses.
An Implantable Cardioverter-Defibrillator is used in patients at risk of life-threatening ventricular arrhythmias. While these devices are not implanted to treat palpitations alone, they provide critical protection when serious rhythms are present.
Treating Anxiety and Symptom Amplification
In many patients, anxiety amplifies the perception of palpitations. Even benign rhythms can feel severe when attention is focused on the heartbeat.
Education, reassurance, and understanding the benign nature of the symptoms—once confirmed—are often as important as medical treatment. Addressing anxiety reduces symptom intensity and improves overall well-being.
Living With Heart Palpitations
Most people experience palpitations at some point in their lives. For many, they are occasional and harmless. For others, they may recur and require evaluation.
The key is not to ignore symptoms, but also not to assume the worst. With appropriate assessment and individualized management, palpitations can usually be explained, controlled, or treated effectively.
In Summary
Heart palpitations are the sensation of being aware of your heartbeat. While they can feel alarming, most palpitations are benign and related to common triggers or extra beats. In some cases, they signal an underlying heart rhythm disorder that requires attention. Proper evaluation allows reassurance when appropriate and targeted treatment when needed.
Reference: Palpitation