Pulmonary embolism is a potentially life-threatening condition that occurs when a blood clot blocks one or more arteries in the lungs. Most pulmonary emboli originate from clots that form in the deep veins of the legs and travel to the lungs through the bloodstream.
Pulmonary embolism can develop suddenly and range from mild to severe. Early recognition and prompt treatment are critical, as PE can place sudden strain on the heart and reduce oxygen levels in the body.
How Pulmonary Embolism Develops
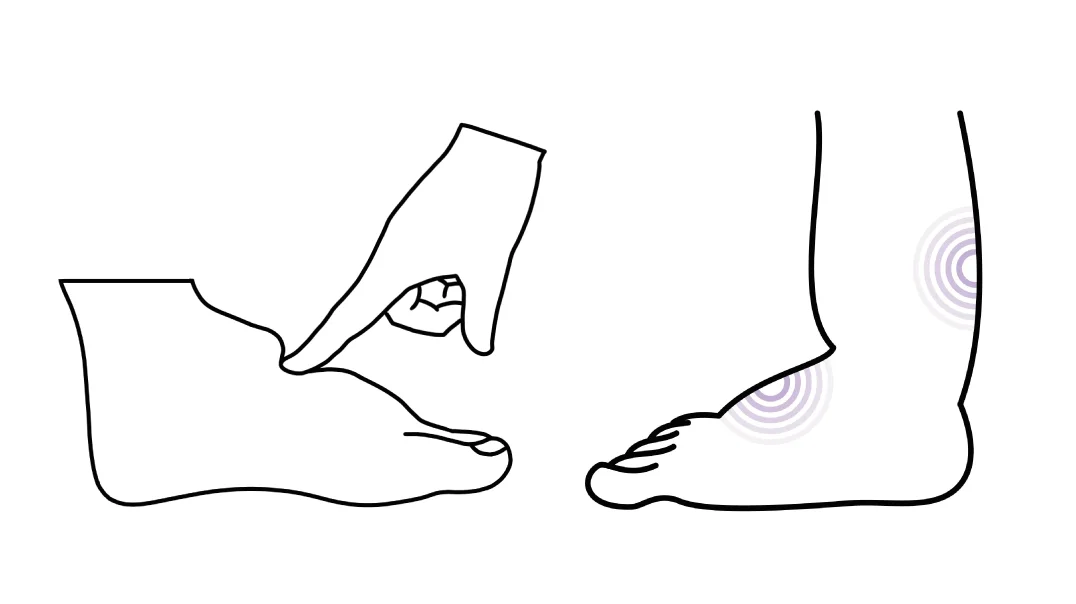
In most cases, pulmonary embolism begins with a clot in the deep veins of the legs or pelvis, a condition known as deep vein thrombosis (DVT). When part or all of this clot breaks free, it can travel to the lungs and lodge in a pulmonary artery.
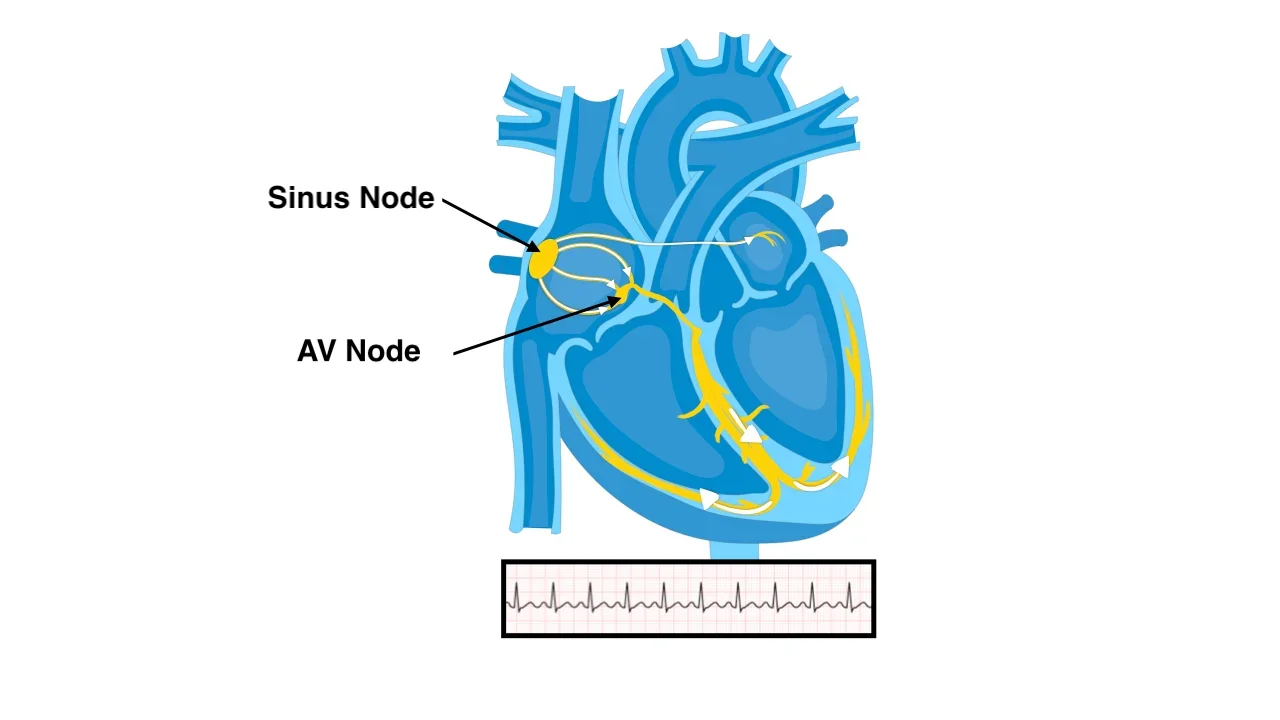
Once the artery is blocked, blood flow to part of the lung is reduced or stopped. This interferes with oxygen exchange and increases pressure in the lung circulation. In larger or multiple clots, the right side of the heart may struggle to pump against this sudden resistance.
Why Pulmonary Embolism Is Dangerous
Pulmonary embolism can impair oxygen delivery to vital organs and place acute strain on the heart. Large or untreated clots may lead to heart failure, shock, or sudden death.
Even smaller clots can cause significant symptoms and long-term complications if not treated appropriately. Because symptoms vary widely, PE can sometimes be difficult to recognize.
Symptoms of Pulmonary Embolism
Symptoms often begin suddenly but may be subtle in some individuals.
Common symptoms include:
- Sudden shortness of breath
- Sharp chest pain, often worse with deep breathing
- Rapid heart rate
- Cough, sometimes with blood-streaked sputum
- Lightheadedness or fainting
Some patients may also have leg pain or swelling due to an underlying deep vein thrombosis.
Risk Factors for Pulmonary Embolism
Pulmonary embolism is more likely to occur in situations that increase blood clot formation or reduce blood flow.
Risk factors include recent surgery or hospitalization, prolonged immobility (such as long flights or bed rest), cancer, pregnancy, hormone therapy, inherited clotting disorders, and a prior history of blood clots.
In some cases, no clear risk factor is identified.
How Pulmonary Embolism Is Diagnosed
Diagnosis is based on clinical assessment, blood tests, and imaging.
A blood test measuring clot breakdown products may help assess likelihood in low-risk patients. CT pulmonary angiography is the most commonly used imaging test and allows direct visualization of clots in the lung arteries.
Echocardiography may be used to assess strain on the heart in more severe cases. Additional testing helps evaluate oxygen levels and identify associated deep vein thrombosis.
Treatment Options for Pulmonary Embolism
Treatment of pulmonary embolism depends on the size and location of the clot, the severity of symptoms, the effect on heart function, and the patient’s overall risk profile. The primary goals are to prevent clot growth, restore blood flow, reduce strain on the heart, and prevent recurrence.
Anticoagulant Therapy
Anticoagulant medications, commonly referred to as blood thinners, are the mainstay of treatment for most patients with pulmonary embolism.
These medications do not dissolve existing clots, but they prevent new clots from forming and stop existing clots from enlarging. This allows the body’s natural processes to gradually break down the clot over time.
Anticoagulants may be started immediately once pulmonary embolism is suspected and are continued for a defined period based on the underlying cause.
- In cases triggered by a temporary risk factor, treatment is often continued for at least 3 months.
- In unprovoked or recurrent cases, long-term or indefinite therapy may be recommended.
Careful monitoring and adherence to therapy are essential to reduce the risk of recurrence and bleeding complications.
Advanced and Emergency Treatments
In some patients, pulmonary embolism causes severe strain on the heart, low blood pressure, or circulatory collapse. These cases are considered high-risk and require urgent treatment in specialized hospital settings.
Thrombolytic (Clot-Dissolving) Therapy
In life-threatening pulmonary embolism, clot-dissolving medications (thrombolytics) may be used to rapidly break down the clot. These drugs act quickly but carry a higher risk of bleeding, so they are reserved for carefully selected patients with severe disease.
Catheter-Based Interventions
In selected cases, catheter-directed therapies may be performed. Using thin tubes inserted through blood vessels, specialists can deliver medication directly to the clot or mechanically remove part of the clot. These approaches aim to reduce clot burden while limiting systemic side effects.
Surgical Embolectomy
Rarely, when other treatments are ineffective or contraindicated, surgical removal of the clot (embolectomy) may be necessary. This is performed in highly specialized centers and is reserved for the most severe cases.
Hospitalization and Monitoring
Patients with moderate to severe pulmonary embolism are typically hospitalized for close monitoring. Heart function, oxygen levels, and response to treatment are carefully assessed, especially during the early phase of therapy.
Repeat imaging or cardiac evaluation may be used to track recovery in selected patients.
Recovery and Duration of Treatment
Recovery from pulmonary embolism varies. Many patients experience gradual improvement in breathing and exercise tolerance over weeks to months.
Long-term follow-up is important to assess:
- Resolution of symptoms
- Risk of recurrence
- Development of chronic complications affecting lung circulation
Treatment duration and preventive strategies are individualized based on these factors.
When to Seek Emergency Care
Sudden unexplained shortness of breath, chest pain, fainting, or coughing up blood should be treated as medical emergencies. Prompt evaluation can be life-saving.
In Summary
Most cases of pulmonary embolism are treated effectively with anticoagulant therapy alone. In severe or life-threatening cases, advanced treatments such as clot-dissolving medications, catheter-based interventions, or surgery may be required. Early diagnosis, appropriate risk-based treatment, and careful follow-up are essential to achieving the best outcomes.
Reference: Pulmonary Embolism