Blood thinners are medications that prevent clot formation in blood vessels, thereby reducing the risk of life-threatening conditions such as heart attack, stroke, and pulmonary embolism. They play a lifesaving role particularly in patients with heart rhythm disorders, heart valve disease, vascular occlusion, or an increased tendency for clotting.
These medications do not actually “thin” the blood. Instead, they suppress the clotting mechanism, preventing the formation of new clots and the growth of existing ones. When used correctly, they are highly effective and safe.
What are blood thinners?
Blood thinners are medications that inhibit the blood clotting process or prevent platelets from sticking together. In this way, unwanted clot formation within blood vessels is prevented.
They are divided into two main groups: anticoagulants and antiplatelet agents. Anticoagulants suppress clotting factors, while antiplatelet agents prevent platelets (blood cells responsible for clot formation) from aggregating.
What do blood thinners do?
Blood thinners prevent clot formation in the heart or blood vessels and reduce the risk of clots traveling to vital organs such as the brain, heart, or lungs.
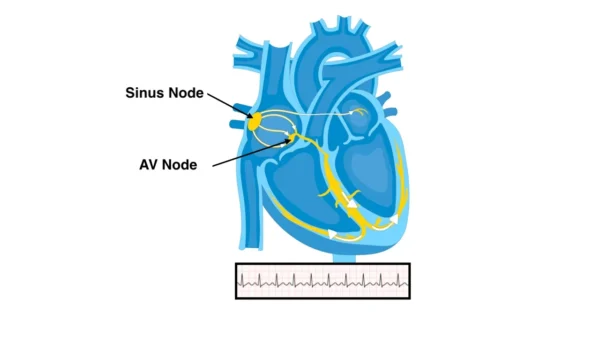
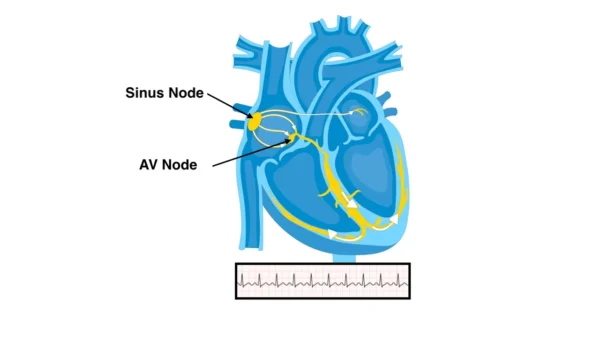
Their most common indications include atrial fibrillation, deep vein thrombosis, pulmonary embolism, prosthetic heart valves, the period after a heart attack, and patients with coronary stents. In these conditions, blood-thinning therapy significantly reduces the risk of stroke and sudden death.
Types of blood thinners
Blood-thinning medications are classified into several groups based on their mechanism of action.
Antiplatelet agents prevent platelet aggregation. Aspirin and clopidogrel are the most well-known examples. They are commonly used after heart attacks, following stent placement, and in patients with atherosclerosis.
Traditional anticoagulants inhibit clotting factors. Warfarin is the most well-known example and requires regular blood monitoring.
Direct oral anticoagulants (DOACs) have more predictable effects and usually do not require routine blood testing. This group includes apixaban, rivaroxaban, dabigatran, and edoxaban.
Injectable anticoagulants are typically used in hospital settings or for temporary protection. Low-molecular-weight heparin is the most common example.
Who needs blood thinners?
Blood thinners are prescribed to patients at high risk of clot formation. Common indications include atrial fibrillation, previous stroke, prosthetic heart valves, blood clots in the leg veins, pulmonary embolism, prolonged immobility, and certain inherited clotting disorders.
Antiplatelet agents are also used in patients with coronary stents to prevent stent thrombosis.
Important precautions
These medications must be taken regularly and at the same time each day. Skipping doses or irregular use significantly increases the risk of clot formation.
Before any surgical procedure, dental extraction, or endoscopy, the physician must be informed. In some cases, blood thinners may need to be temporarily discontinued.
Patients should seek medical attention if they notice easy bruising, nosebleeds, gum bleeding, or blood in the urine or stool.
Side effects
The most important side effect is bleeding. This can range from minor bruising to life-threatening internal bleeding.
Dizziness, fatigue, gastrointestinal discomfort, and rarely allergic reactions may also occur. However, with appropriate dosing and regular follow-up, the risk of serious side effects is relatively low.
Nutrition while using blood thinners
In patients taking warfarin, intake of foods rich in vitamin K should be consistent and balanced. Sudden increases in consumption of green leafy vegetables may reduce the effectiveness of the medication.
New-generation blood thinners do not have significant interactions with foods. However, alcohol consumption can increase bleeding risk in all groups.
Duration of treatment
The duration of therapy depends on the underlying condition. In temporary risk situations, treatment for 3–6 months may be sufficient, whereas lifelong therapy may be required in patients with atrial fibrillation or mechanical heart valves.
The treatment duration must always be determined by a physician.
What happens if blood thinners are stopped?
Abrupt discontinuation of blood thinners leads to a rapid increase in clotting risk. This can result in serious outcomes such as stroke, heart attack, or pulmonary embolism.
For this reason, stopping or changing the dose without medical advice is extremely dangerous.
Important warning
If you are using blood thinners and experience uncontrolled bleeding, a sudden increase in bruising, severe headache, fainting, or blood in the urine or stool, you should seek immediate medical attention.
Reference: Anticoagulation