A heart attack, medically known as myocardial infarction, occurs when blood flow to a part of the heart muscle is suddenly blocked, depriving the tissue of oxygen. Without prompt treatment, the affected heart muscle begins to suffer irreversible damage.
Heart attack is a medical emergency. Early recognition and rapid treatment are critical and can be life-saving, significantly reducing heart muscle damage and long-term complications.
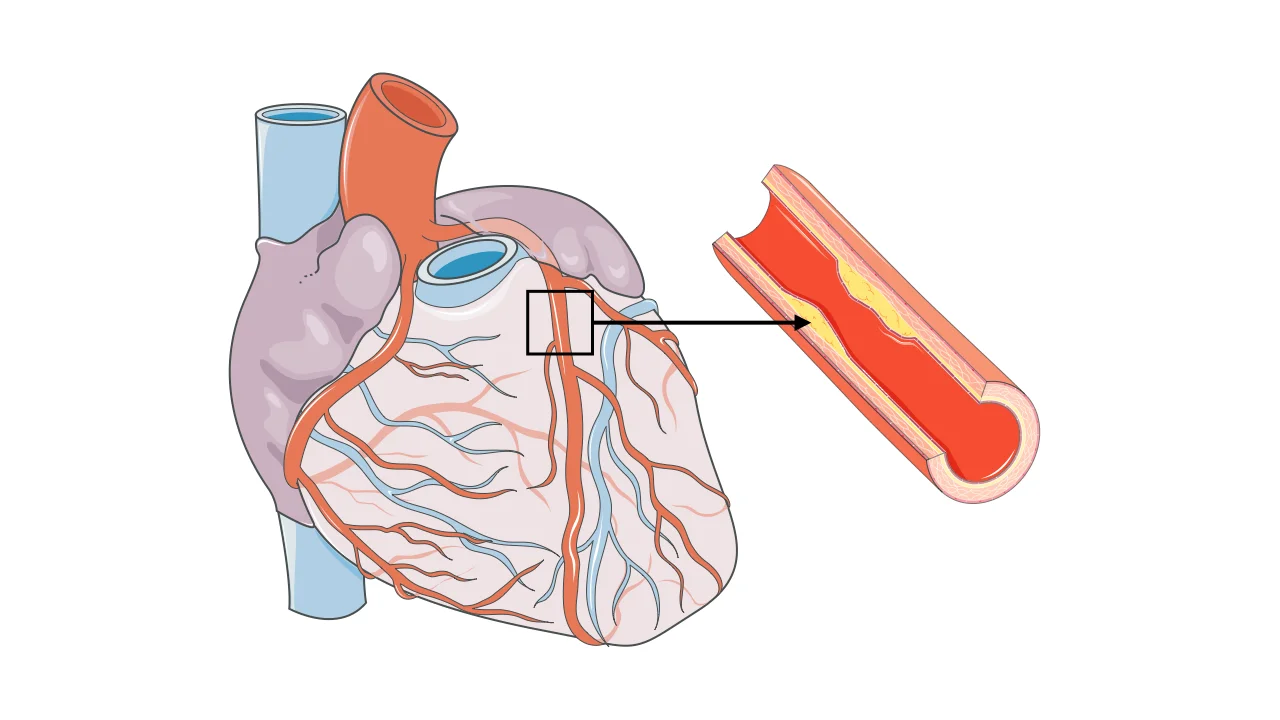
What Happens During a Heart Attack?
Most heart attacks are caused by atherosclerosis, a process in which cholesterol-rich plaques build up inside the coronary arteries. When a plaque ruptures, a blood clot can rapidly form and completely block blood flow to part of the heart.
The longer the blockage persists, the greater the damage to the heart muscle. This is why heart attack treatment focuses on restoring blood flow as quickly as possible.
Common Symptoms of a Heart Attack
Heart attack symptoms can vary widely and do not always appear suddenly or dramatically.
Typical symptoms include:
- Chest pain, pressure, tightness, or a squeezing sensation
- Pain radiating to the arm, shoulder, neck, jaw, or back
- Shortness of breath
- Cold sweats
- Nausea or vomiting
- Unusual fatigue or weakness
Some people—particularly women, older adults, and individuals with diabetes—may experience atypical symptoms, such as shortness of breath, fatigue, or indigestion-like discomfort rather than classic chest pain.
When to Seek Emergency Care
Any new, persistent chest discomfort or symptoms suggestive of a heart attack should prompt immediate emergency medical attention. Waiting for symptoms to pass can result in permanent heart damage or death.
Early treatment saves heart muscle.
Causes and Risk Factors
The most common cause of heart attack is coronary artery disease. Several factors increase the risk:
- High LDL cholesterol
- High blood pressure
- Smoking
- Diabetes
- Obesity and physical inactivity
- Family history of heart disease
- Chronic stress
Addressing these risk factors plays a key role in prevention.
How a Heart Attack Is Diagnosed
Diagnosis is based on a combination of symptoms, electrocardiography (ECG), and blood tests measuring cardiac enzymes that indicate heart muscle injury.
Imaging studies and coronary angiography are often used to identify the blocked artery and guide treatment.
Treatment of a Heart Attack
Heart attack treatment focuses on rapid restoration of blood flow, limiting heart muscle damage, and preventing complications.
Emergency and Acute Treatment
Immediate treatment may include oxygen, medications to relieve pain and prevent clot growth, and rapid transfer to a cardiac care unit.
The most effective treatment for many heart attacks is urgent coronary angiography followed by angioplasty and stent placement, a procedure that opens the blocked artery and restores blood flow.
In situations where catheter-based treatment is not immediately available, clot-dissolving medications may be used in selected patients.
Hospital Care and Monitoring
After blood flow is restored, patients are closely monitored for heart rhythm disturbances, heart failure, or other complications. Medications are started to protect the heart and reduce the risk of future events.
Recovery After a Heart Attack
Recovery begins in the hospital and continues for months afterward. Cardiac rehabilitation programs play a crucial role by combining supervised exercise, education, and lifestyle guidance.
Most people can return to active, productive lives with appropriate treatment and follow-up.
Preventing Another Heart Attack
Preventive strategies focus on controlling risk factors and protecting the heart long term.
These include:
- Cholesterol-lowering therapy
- Blood pressure control
- Smoking cessation
- Heart-healthy nutrition
- Regular physical activity
- Stress management
Medications prescribed after a heart attack are often lifelong and are essential for reducing recurrence risk.
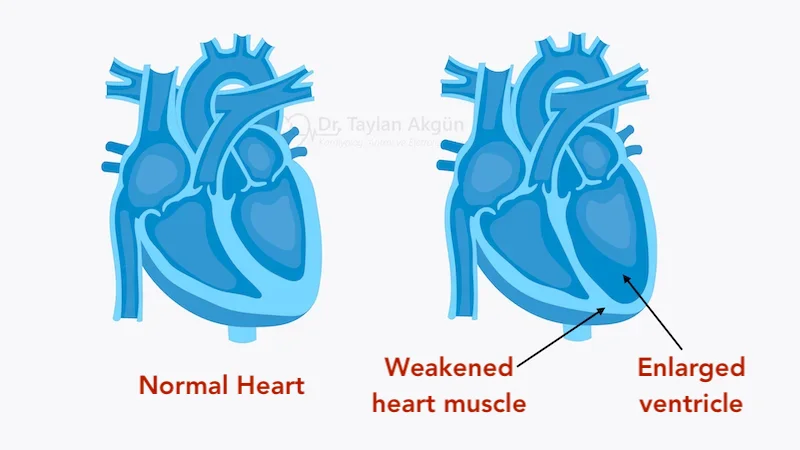
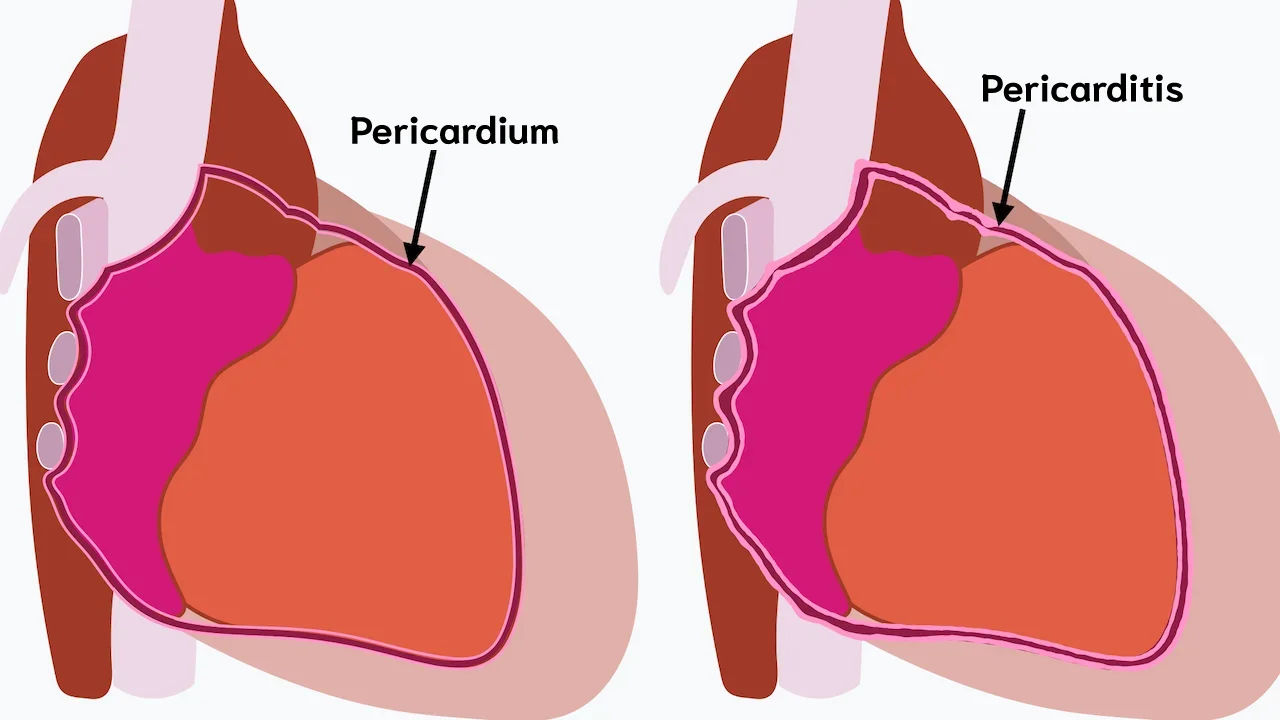
Possible Complications
Heart attacks can lead to complications such as heart failure, abnormal heart rhythms, or reduced pumping function. Early treatment and close follow-up significantly reduce these risks.
In Summary
A heart attack occurs when blood flow to the heart muscle is suddenly blocked, most often due to plaque rupture and clot formation. Symptoms may vary, but prompt recognition and emergency treatment are critical. With modern therapies, early intervention, and long-term risk factor management, many people recover well and significantly reduce their risk of future heart attacks.
Reference: Myocardial Infarction