An implantable cardioverter defibrillator (ICD) is a small electronic device implanted under the skin to continuously monitor heart rhythm and immediately treat life-threatening arrhythmias. Its primary purpose is to prevent sudden cardiac death by rapidly terminating dangerous rhythms that arise from the ventricles, often before the patient loses consciousness.
Unlike standard pacemakers, which are designed mainly to support slow heart rates, an ICD is focused on detecting and stopping malignant fast rhythms. In selected patients, it also provides pacing support when needed, but its defining role is protection against fatal arrhythmias.
What an ICD Does—In Real Life
An ICD constantly analyzes every heartbeat. If it detects a dangerous rhythm such as ventricular tachycardia or ventricular fibrillation, it responds automatically. For some fast but organized rhythms, the device may first deliver painless rapid pacing to interrupt the arrhythmia. If the rhythm is chaotic or unstable, the ICD delivers a defibrillation shock to immediately restore a safe rhythm.
All of this happens within seconds, without the patient needing to take any action. Many patients are unaware the device has intervened until symptoms resolve or the event is later reviewed during device follow-up.
Who Benefits From an Implantable Cardioverter Defibrillator?
ICD therapy is considered for patients who have already experienced, or are at high risk of developing, life-threatening ventricular arrhythmias. This includes people who have survived sudden cardiac arrest, those with documented ventricular tachycardia or fibrillation, and selected patients with significantly weakened heart muscle due to heart failure or cardiomyopathy.
Certain inherited electrical or structural heart conditions also carry an increased risk of sudden death. In these situations, an ICD may be recommended even before a life-threatening rhythm has occurred, based on careful risk assessment. Long QT syndrome, Brugada syndrome, and arrhythmogenic right ventricular cardiomyopathy are genetic conditions that affect the heart’s electrical system and may require ICD protection.
The decision to implant an ICD is never based on heart rate alone. It reflects an individualized evaluation of arrhythmia risk, overall health, life expectancy, and expected benefit.
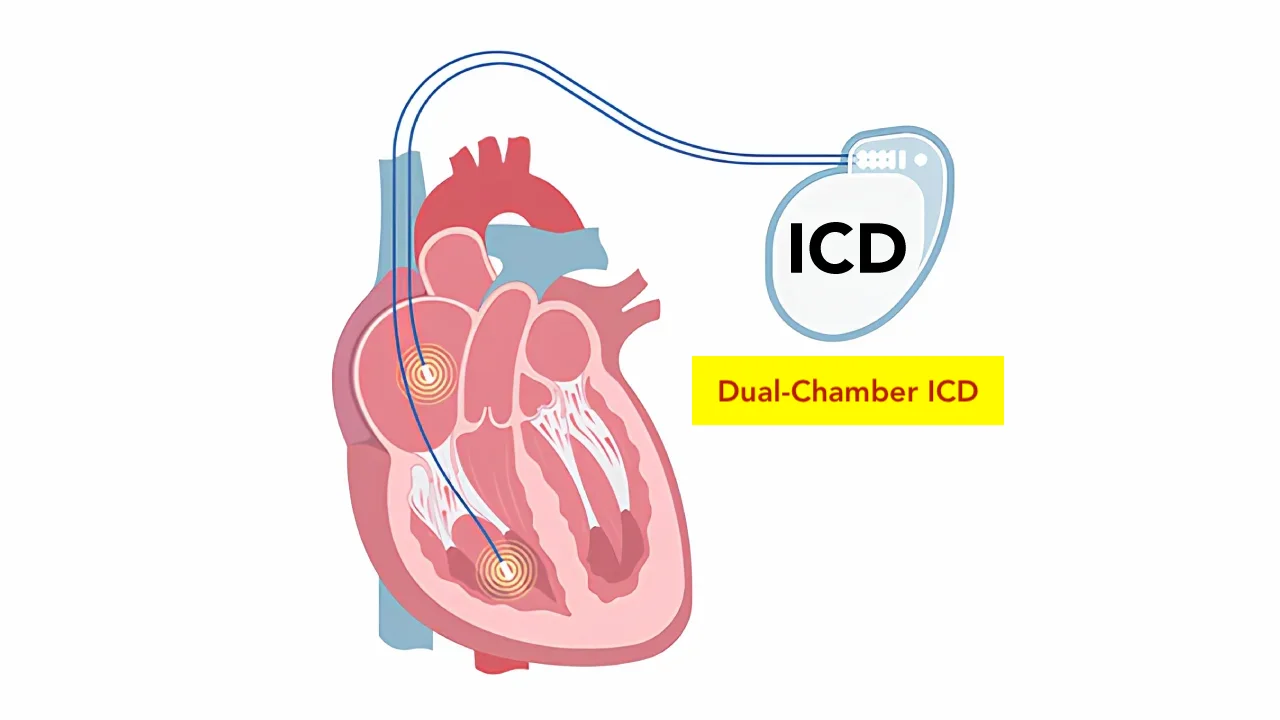
Types of ICD Systems
The most commonly used ICD system places one or more leads through the veins into the heart, allowing accurate rhythm detection, pacing, and shock delivery. This approach is suitable for the majority of patients and allows the greatest flexibility in therapy.
In selected individuals who do not need pacing support, a subcutaneous ICD may be used. In this system, the device and lead are placed entirely under the skin, avoiding contact with the heart and blood vessels. This option can be particularly attractive for younger patients or those at higher risk of bloodstream infection.
Some patients with heart failure require both defibrillation protection and resynchronization of heart contractions. In these cases, a combined system known as CRT-D provides biventricular pacing together with ICD therapy.
The ICD Implantation Procedure
ICD implantation is a minimally invasive procedure performed in a cardiac electrophysiology laboratory. It is usually done under local anesthesia with light sedation.
A small incision is made below the collarbone, and the ICD lead or leads are guided into position using imaging. Once placement is confirmed and tested, the device is connected and positioned under the skin. The system is then programmed according to the patient’s specific arrhythmia profile.
The procedure typically lasts one to two hours. Most patients are able to sit up shortly afterward and are discharged within one or two days.
Recovery and Life After ICD Implantation
Recovery from ICD implantation is generally straightforward. Temporary soreness or bruising near the device site is common and improves within days. During the first few weeks, patients are advised to avoid heavy lifting or extreme arm movements on the implantation side to allow proper healing.
Living with an ICD usually requires minimal lifestyle adjustment. Modern devices are compatible with most daily activities and household electronics. Regular follow-up visits—or remote monitoring—are essential to check battery status, review stored rhythm events, and fine-tune device settings.
Battery life typically ranges from six to ten years. When replacement is needed, the generator can usually be exchanged without removing the leads.
Understanding ICD Shocks
An ICD shock can be startling or uncomfortable, but it is delivered only when a potentially fatal rhythm is detected. In that moment, the shock is life-saving. Advances in device programming have greatly reduced unnecessary shocks, favoring painless therapies whenever possible.
Any ICD shock should prompt medical review, not because the device has failed, but to understand what triggered the arrhythmia and whether treatment adjustments are needed.
Safety, Risks, and Limitations
ICD implantation is a well-established and generally safe procedure. As with any implanted device, potential complications include infection, lead-related issues, or inappropriate therapy, though these are uncommon with modern techniques and follow-up.
It is also important to recognize that an ICD does not prevent arrhythmias from occurring. Instead, it prevents arrhythmias from becoming fatal, acting as a continuous safety net.
In Summary
An implantable cardioverter defibrillator is a life-saving device that continuously monitors heart rhythm and rapidly treats dangerous ventricular arrhythmias. ICD therapy is reserved for patients with significant risk of sudden cardiac death and is based on careful, individualized assessment. With modern devices, expert implantation, and regular follow-up, ICDs provide long-term protection while allowing patients to live active, meaningful lives.
Reference: ICD