Ventricular tachycardia, often abbreviated as VT, is a fast heart rhythm that originates in the lower chambers of the heart, called the ventricles. Because the ventricles are responsible for pumping blood to the entire body, rhythms that start here are taken more seriously than many other arrhythmias.
VT can range from brief, self-limited episodes to sustained, life-threatening rhythms that require urgent medical attention. Understanding what VT is—and what it is not—helps patients and families respond appropriately without unnecessary panic.
- How Ventricular Tachycardia Affects the Heart
- Symptoms of Ventricular Tachycardia
- Why Ventricular Tachycardia Occurs
- Types of Ventricular Tachycardia
- Is Ventricular Tachycardia Dangerous?
- How Ventricular Tachycardia Is Diagnosed
- Treatment Options for Ventricular Tachycardia
- Living With Ventricular Tachycardia
- In Summary
How Ventricular Tachycardia Affects the Heart
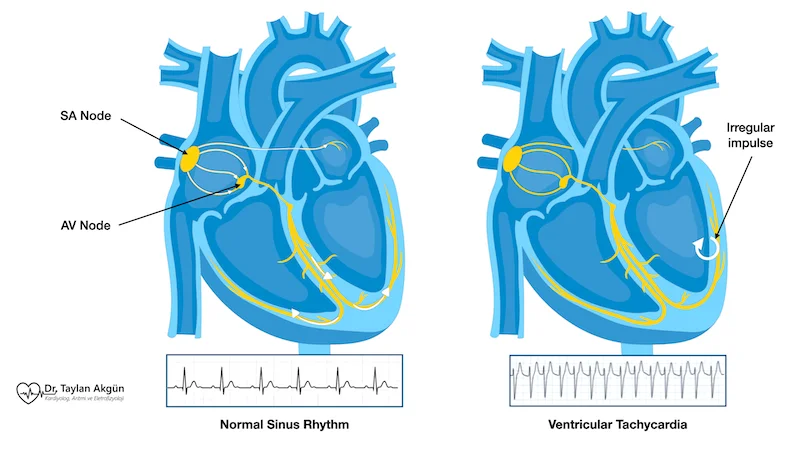
In a normal heartbeat, electrical signals travel in an organized sequence that allows the ventricles to fill with blood before contracting. In ventricular tachycardia, abnormal electrical signals arise directly within the ventricular muscle.
Because the heart is beating very fast, it has little time to fill between beats. As a result, less blood is pumped with each contraction. This reduction in blood flow can quickly affect the brain and other vital organs, explaining why VT often causes significant symptoms.
Unlike many supraventricular rhythms, VT interferes directly with the heart’s main pumping chambers.
Symptoms of Ventricular Tachycardia
The symptoms of VT depend on how fast the rhythm is, how long it lasts, and whether there is underlying heart disease.
Some episodes are brief and cause only mild symptoms. Others are sustained and lead to severe instability.
Common symptoms include:
- Sudden onset of rapid heartbeat
- Palpitations that feel strong or forceful
- Dizziness or lightheadedness
- Shortness of breath
- Chest discomfort
- Fainting or near-fainting
In severe cases, VT can cause collapse or cardiac arrest and requires immediate emergency care.
Why Ventricular Tachycardia Occurs
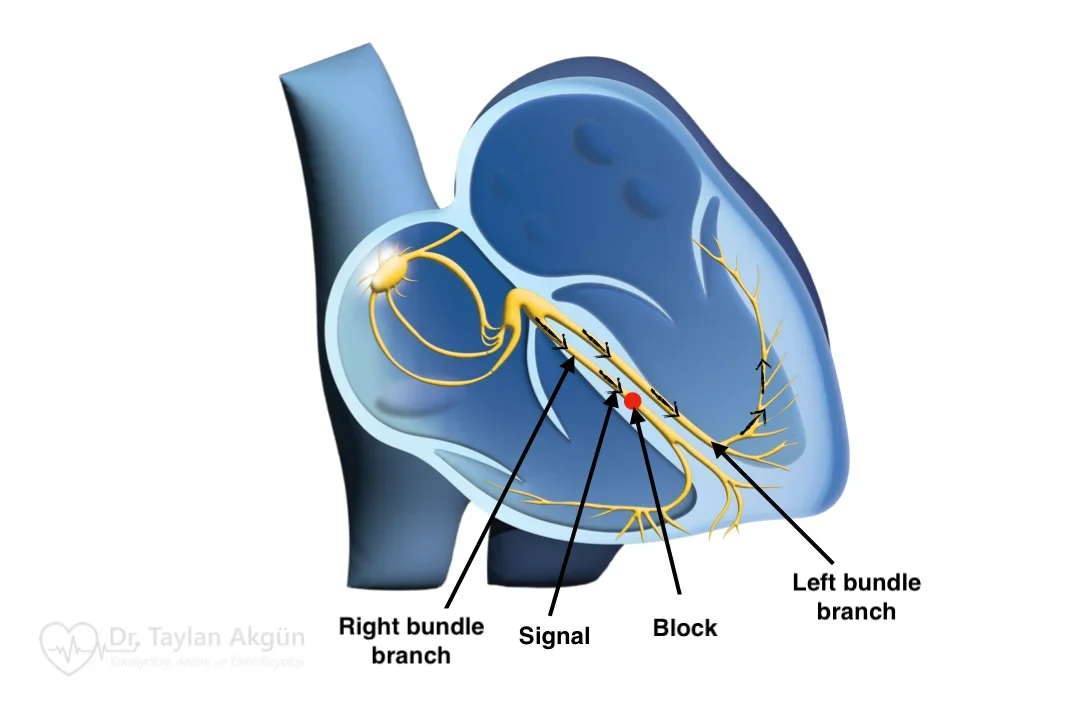
Ventricular tachycardia most often develops in hearts that have been structurally damaged. Scar tissue from a prior heart attack is one of the most common causes. This scar can disrupt normal electrical conduction and create pathways that allow abnormal rhythms to persist.
Other causes include cardiomyopathies, inherited heart muscle diseases, inflammation of the heart muscle, electrolyte imbalances, and certain medications. In some people—especially younger individuals—VT can occur in hearts that appear otherwise normal.
Identifying the underlying cause is essential because it strongly influences both risk and treatment strategy.
Types of Ventricular Tachycardia
VT is classified based on its electrical pattern and clinical behavior.
- Monomorphic VT has a consistent electrical pattern and is often related to scar tissue in the heart. It tends to be recurrent and predictable.
- Polymorphic VT shows changing electrical patterns and is often associated with acute conditions such as ischemia, electrolyte abnormalities, or inherited electrical disorders.
VT may also be described as non-sustained (lasting seconds and stopping on its own) or sustained (lasting longer and requiring intervention). Sustained VT is generally more dangerous and demands urgent evaluation.
Is Ventricular Tachycardia Dangerous?
This is a critical question—and the answer depends on context.
VT is considered potentially life-threatening, especially when it is sustained or occurs in the presence of structural heart disease. It can deteriorate into more unstable rhythms and compromise circulation.
That said, not all VT is immediately fatal. Some forms are stable and manageable, particularly when recognized early and treated appropriately. This is why careful risk assessment is essential rather than assuming all VT behaves the same way.
How Ventricular Tachycardia Is Diagnosed
Diagnosis requires documenting the rhythm, usually with an electrocardiogram. Because VT may occur unpredictably, prolonged rhythm monitoring or implanted recorders may be used.
Imaging tests evaluate heart structure and function, while additional studies help determine whether scar tissue, ischemia, or inherited conditions are present.
The diagnostic process focuses on identifying the cause, the risk of recurrence, and the risk of sudden cardiac events.
Treatment Options for Ventricular Tachycardia
Treatment of VT is guided by severity, underlying heart disease, and overall risk.
Medications may be used to suppress abnormal rhythms or reduce recurrence. In acute settings, electrical cardioversion may be required to restore a stable rhythm.
For many patients at significant risk, an Implantable Cardioverter-Defibrillator is recommended. This device continuously monitors the heart rhythm and can deliver life-saving therapy if VT occurs.
In selected patients, catheter ablation may be performed to target and eliminate the abnormal electrical circuits responsible for VT. This procedure can reduce the frequency of episodes and improve quality of life but is often used alongside other protective strategies rather than as a standalone cure.
Living With Ventricular Tachycardia
A diagnosis of VT can be frightening. Education and clear communication are essential to help patients understand their specific risk and treatment plan.
With modern therapies, including medications, ablation, and implantable devices, many people with VT are able to live active and meaningful lives. Ongoing follow-up and adherence to treatment recommendations are crucial.
In Summary
Ventricular tachycardia is a fast heart rhythm originating in the ventricles and carries a higher risk than many other arrhythmias. While some forms are stable and manageable, others can be life-threatening. Accurate diagnosis, careful risk assessment, and individualized treatment allow VT to be managed safely and effectively in most patients.
Reference: Ventricular Tachycardia