What is Dressler syndrome?
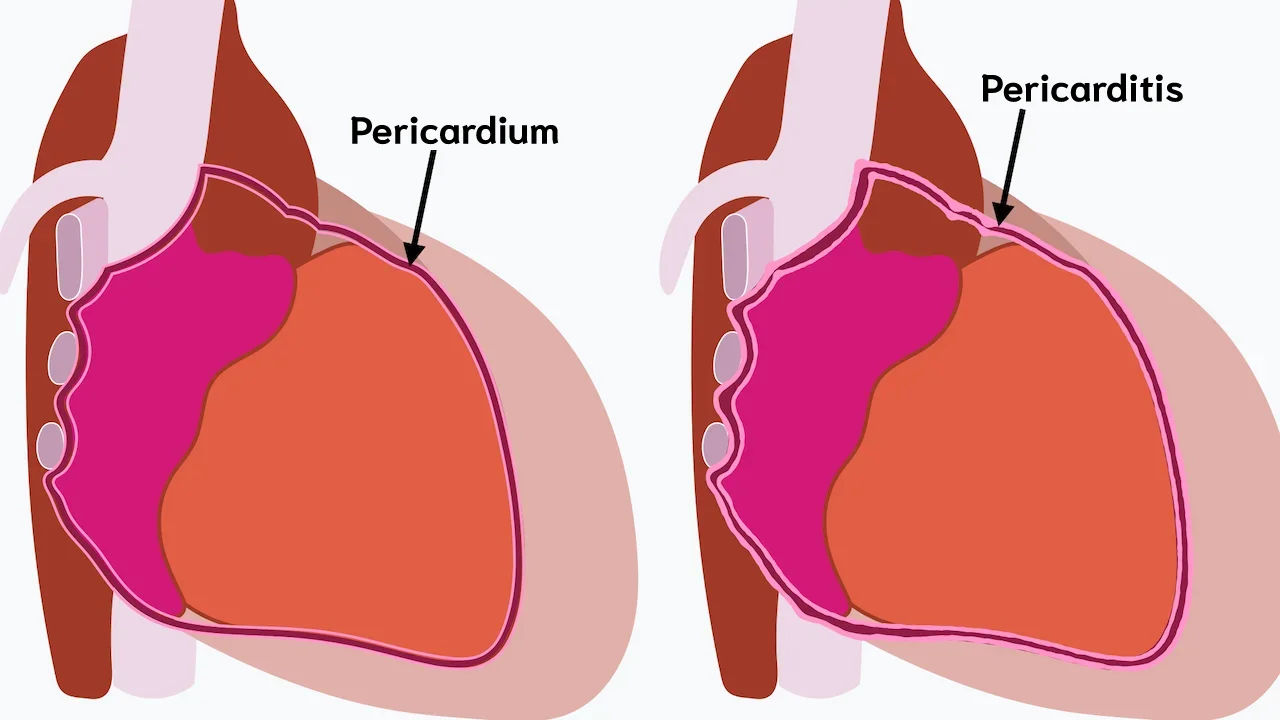
Dressler syndrome is a type of inflammatory reaction that affects the pericardium, the thin sac surrounding the heart. It typically develops weeks to months after an injury to the heart muscle. The most common trigger is a heart attack, but it can also occur after cardiac surgery, trauma, or other forms of heart injury.
Dressler syndrome is considered a form of post-cardiac injury syndrome and is thought to be immune-mediated rather than caused by direct infection.
Unlike early post–heart attack pericarditis, which occurs within days, Dressler syndrome usually appears 2–8 weeks after the cardiac injury, though it can develop later.
Symptoms of Dressler syndrome
Symptoms usually develop gradually and may vary in severity.
Common symptoms include:
- Chest pain (often sharp and pleuritic, worse with deep breathing or lying flat)
- Low-grade fever
- Shortness of breath
- Fatigue and malaise
- Pericardial friction rub (heard on physical examination)
Chest pain often improves when sitting up or leaning forward, which is typical of pericardial inflammation.
When to seek medical attention
Medical evaluation is important if you experience:
- New or worsening chest pain after a heart attack or heart surgery
- Fever without an obvious source
- Increasing shortness of breath
- Symptoms suggesting fluid accumulation around the heart
Early assessment helps distinguish Dressler syndrome from more serious conditions such as recurrent myocardial infarction or infection.
What causes Dressler syndrome?
The exact mechanism is not fully understood, but Dressler syndrome is believed to result from an autoimmune response triggered by myocardial injury.
Common causes include:
- Heart attack (Myocardial infarction)
- Cardiac surgery (such as coronary artery bypass or valve surgery)
- Cardiac trauma
- Percutaneous coronary interventions (rarely)
- Myocarditis or other forms of myocardial injury
Damage to heart tissue releases intracellular components, which the immune system mistakenly recognizes as foreign, leading to inflammation.
Possible complications
Most cases are mild and self-limited, but complications can occur.
Potential complications include:
- Pericardial effusion (fluid around the heart)
- Pleural effusion
- Cardiac tamponade (rare but life-threatening)
- Recurrent pericarditis
Early recognition and treatment significantly reduce the risk of complications.
How is Dressler syndrome diagnosed?
Diagnosis is based on clinical presentation and supportive findings rather than a single definitive test.
Evaluation may include:
- Medical history showing recent cardiac injury
- Physical examination (pericardial rub)
- Electrocardiogram
- Blood tests showing elevated inflammatory markers (CRP, ESR)
- Echocardiography to assess pericardial effusion
- Chest X-ray if pleural involvement is suspected
Infection and recurrent myocardial ischemia must be excluded.
How is Dressler syndrome treated?
Treatment focuses on controlling inflammation and relieving symptoms.
First-line treatment usually includes:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- High-dose aspirin (preferred in post–myocardial infarction patients)
Colchicine may be added to:
- Improve symptom control
- Reduce recurrence risk
Corticosteroids are generally reserved for patients who do not respond to NSAIDs or colchicine, as they may increase recurrence rates if used early.
Prognosis
The prognosis of Dressler syndrome is generally good. Most patients recover fully with appropriate anti-inflammatory treatment.
Recurrence is possible but less common with modern treatment strategies. Long-term outcomes are usually favorable, especially when complications are promptly managed.
Key points to remember
- Dressler syndrome is an immune-mediated form of pericarditis occurring weeks after heart injury
- Chest pain and low-grade fever are common symptoms
- Diagnosis is clinical and supported by imaging and laboratory tests
- Treatment is usually effective and prognosis is good
Reference: Dressler syndrome