Hypertrophic cardiomyopathy (HCM) is a condition in which the heart muscle becomes abnormally thickened, most commonly affecting the left ventricle. This thickening is not caused by high blood pressure or valve disease, but rather by changes within the heart muscle itself—most often due to inherited genetic mutations.
HCM is one of the most common inherited heart diseases. Its presentation varies widely, ranging from individuals who never develop symptoms to those who experience significant limitations or serious rhythm disturbances.
- How Hypertrophic Cardiomyopathy Affects the Heart
- Symptoms of Hypertrophic Cardiomyopathy
- Causes and Genetics
- Hypertrophic Cardiomyopathy and Sudden Cardiac Death
- How Hypertrophic Cardiomyopathy Is Diagnosed
- Treatment Options for Hypertrophic Cardiomyopathy
- Living With Hypertrophic Cardiomyopathy
- In Summary
How Hypertrophic Cardiomyopathy Affects the Heart
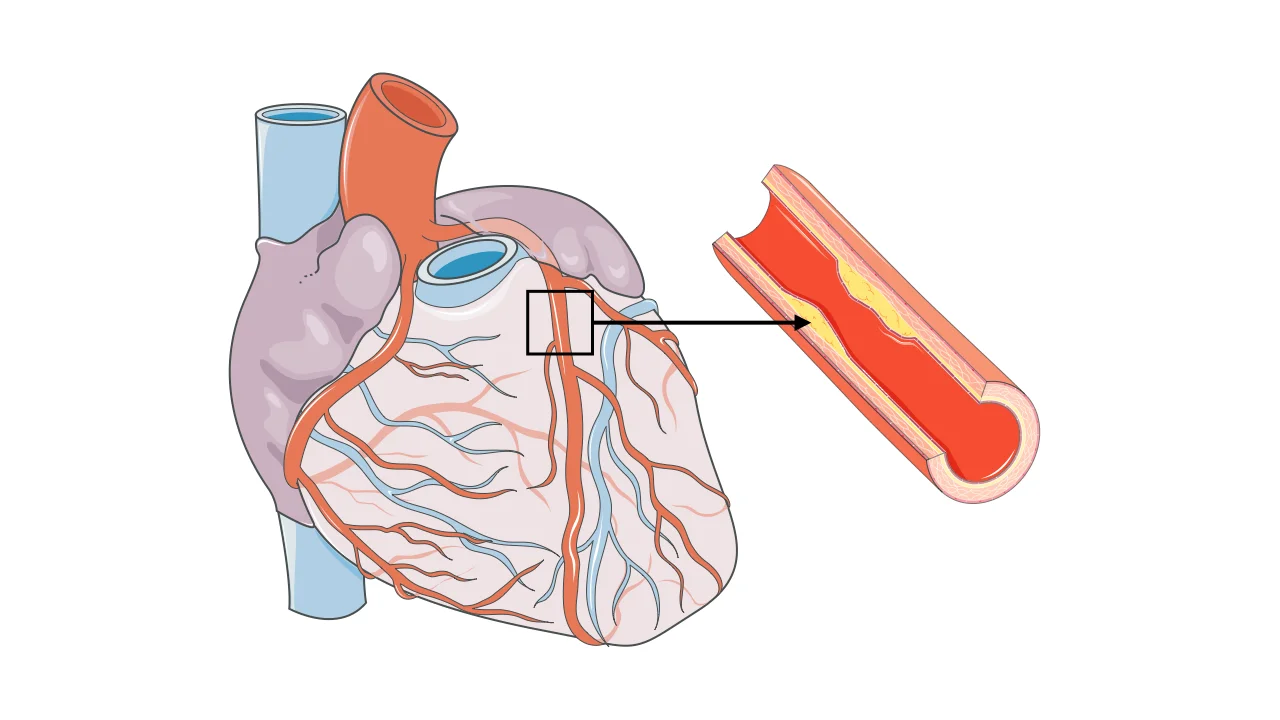
In HCM, the thickened heart muscle may interfere with normal heart function in two main ways. First, the stiff muscle may not relax properly, impairing the heart’s ability to fill with blood between beats. Second, in some patients, the thickened muscle obstructs blood flow as it leaves the heart, a condition known as left ventricular outflow tract obstruction.
These changes increase pressure inside the heart and can reduce blood flow to the body, particularly during physical activity.
Obstructive and Non-Obstructive HCM
Hypertrophic cardiomyopathy is often categorized based on whether blood flow out of the heart is obstructed.
In obstructive HCM, thickened muscle partially blocks blood flow from the left ventricle, especially during exertion. This form is more likely to cause symptoms such as shortness of breath, chest pain, or fainting.
In non-obstructive HCM, the heart muscle is thickened but does not significantly block blood flow. Symptoms may still occur due to impaired filling or abnormal relaxation of the heart.
Symptoms of Hypertrophic Cardiomyopathy
Symptoms may develop gradually or appear suddenly, particularly during physical exertion.
Common symptoms include:
- Shortness of breath with activity
- Chest pain, especially during exercise
- Palpitations
- Dizziness or lightheadedness
- Fainting or near-fainting episodes
Some individuals remain completely asymptomatic and are diagnosed only after family screening or routine testing.
Causes and Genetics
Hypertrophic cardiomyopathy is most often caused by inherited mutations affecting proteins responsible for heart muscle contraction. These mutations are passed down in families, meaning close relatives may also be affected.
Because of this genetic basis, family screening and genetic counseling are important components of HCM care.
Hypertrophic Cardiomyopathy and Sudden Cardiac Death
One of the most serious concerns in HCM is the risk of sudden cardiac death, particularly in younger individuals and athletes. This risk is related to dangerous ventricular arrhythmias (VFib) that may occur unpredictably.
Importantly, not all patients with HCM are at high risk. Careful risk assessment allows identification of individuals who may benefit from preventive strategies.
How Hypertrophic Cardiomyopathy Is Diagnosed
Diagnosis is based on imaging of the heart muscle. Echocardiography is the primary test, allowing visualization of wall thickness, heart function, and the presence of outflow obstruction.
Cardiac MRI provides additional detail, particularly regarding the distribution of hypertrophy and the presence of scar tissue. Genetic testing may be recommended in selected patients and families.
Treatment Options for Hypertrophic Cardiomyopathy
Treatment of hypertrophic cardiomyopathy (HCM) is individualized and depends on symptom severity, the presence and degree of left ventricular outflow tract obstruction, and the risk of dangerous heart rhythm disturbances. The main goals are symptom control, prevention of complications, and reduction of sudden cardiac death risk.
Lifestyle and Activity Recommendations
Lifestyle management is an essential part of HCM care. Physical activity recommendations are tailored to the individual, taking into account symptoms, obstruction, and arrhythmia risk.
Many patients are encouraged to remain physically active at a moderate level, while high-intensity or competitive sports may be restricted, particularly in those with significant obstruction or high arrhythmic risk. Adequate hydration, avoidance of excessive alcohol, and careful use of medications that lower blood pressure or cause dehydration are important.
Because HCM is often inherited, family screening and genetic counseling are strongly recommended.
Medication Therapy
Medications are the first-line treatment for most symptomatic patients. These drugs help slow the heart rate, improve relaxation of the heart muscle, and reduce obstruction during exertion.
By improving filling and reducing the force of contraction, medications can significantly relieve symptoms such as shortness of breath, chest pain, and palpitations. While medications improve symptoms, they do not reverse the underlying muscle thickening and require ongoing follow-up and dose adjustment.
Septal Reduction Procedures for Obstructive HCM
In patients with obstructive HCM who remain symptomatic despite optimal medical therapy, procedures aimed at reducing the thickness of the septal muscle may be considered. These treatments are collectively referred to as septal reduction therapy.
One option is surgical septal myectomy, an open-heart procedure in which excess thickened muscle is carefully removed to widen the outflow tract. This operation is highly effective when performed in experienced centers and often provides long-term symptom relief.
Another option in selected patients is alcohol septal ablation, a catheter-based procedure in which a small amount of alcohol is injected into a targeted heart muscle branch artery to reduce muscle thickness in a controlled manner. This approach avoids open-heart surgery and may be appropriate for carefully selected individuals.
The choice between these procedures depends on anatomy, age, symptoms, and center expertise.
Implantable Defibrillator (ICD) Therapy
Some individuals with HCM are at increased risk of life-threatening ventricular arrhythmias and sudden cardiac death. In these patients, implantation of an Implantable Cardioverter-Defibrillator may be recommended.
An ICD continuously monitors heart rhythm and can immediately treat dangerous arrhythmias if they occur. ICD therapy does not treat symptoms or obstruction, but it plays a critical role in preventing sudden cardiac death in high-risk patients.
Long-Term Follow-Up and Reassessment
HCM is a lifelong condition that can change over time. Regular follow-up allows reassessment of symptoms, obstruction severity, and arrhythmia risk. Treatment plans are adjusted as the disease evolves and as new therapies become available.
Shared decision-making between patients and experienced care teams is central to successful long-term management.
Living With Hypertrophic Cardiomyopathy
Many people with HCM live long and active lives with appropriate monitoring and treatment. Regular follow-up is essential to reassess symptoms, heart structure, and arrhythmia risk over time.
Education, family evaluation, and shared decision-making play central roles in successful long-term management.
In Summary
Treatment of hypertrophic cardiomyopathy combines lifestyle guidance, medications, and—when necessary—advanced procedures such as septal myectomy or alcohol septal ablation. In patients at increased arrhythmic risk, ICD therapy provides life-saving protection. With individualized care and expert follow-up, most people with HCM can achieve good symptom control and maintain an active, fulfilling life.
You may also like to read these:
Reference: Hypertrophic cardiomyopathy