Chest pain is one of the most frightening symptoms you can experience. Your first thought might be heart attack, and while that’s certainly possible, chest pain has many causes—some serious, others not. The pain might come from your heart, lungs, digestive system, muscles, ribs, or even anxiety. It can feel like crushing pressure, sharp stabbing, burning, or dull aching. It might last seconds or hours, stay in one spot or spread to your arms, neck, or back. But chest pain from heartburn, muscle strain, or panic attacks can sometimes feel surprisingly similar, which is why proper evaluation is crucial when chest pain occurs.
Overview
Chest pain means any discomfort or pain you feel anywhere in your chest, from your neck down to your upper abdomen. It ranges from harmless to life-threatening.
Your chest contains many organs and structures—your heart, lungs, esophagus (the tube connecting your mouth to your stomach), major blood vessels, ribs, muscles, and nerves. Problems with any of these can cause chest pain.
Heart-related causes are what worry people most. A heart attack occurs when a coronary artery becomes completely blocked, cutting off blood flow to part of your heart muscle. This typically causes intense pressure or squeezing in the center of your chest. Angina is chest discomfort from temporarily inadequate blood flow to your heart, usually during exertion. Problems with the aorta—your body’s main artery—can cause severe, tearing chest or back pain.
Lung-related causes include blood clots in lung arteries, collapsed lungs, pneumonia, or inflammation of the lining around your lungs.
Digestive causes are surprisingly common. Heartburn from stomach acid backing up into your esophagus can cause burning chest pain that mimics heart problems. Esophageal spasms cause sudden, severe chest pain. Gallbladder problems cause pain in the upper right chest or abdomen.
Musculoskeletal causes include strained chest muscles, inflamed rib cartilage, or injured ribs. These cause pain that worsens with movement or pressing on the area.
Panic attacks cause chest tightness, rapid heartbeat, shortness of breath, and intense fear. The symptoms can feel identical to heart attacks.
The key is recognizing which chest pain needs immediate emergency care versus which can wait for a regular appointment.
When to Seek Emergency Care
Some chest pain requires immediate emergency care. Don’t wait or try to drive yourself—contact emergency services or go to the nearest emergency department immediately.
- Seek emergency care if your chest pain feels like pressure, squeezing, fullness, or tightness in the center of your chest lasting more than a few minutes. This is particularly urgent if the pain spreads to your arms, neck, jaw, back, or stomach.
- Seek emergency care if chest pain comes with shortness of breath, sweating, nausea, lightheadedness, or feeling like you might pass out.
- Seek emergency care if you have sudden, severe chest pain that feels like tearing or ripping, especially if it radiates to your back. This suggests aortic dissection—a life-threatening emergency.
- Seek emergency care if you have sharp chest pain with sudden shortness of breath, especially after long periods of sitting, recent surgery, or long travel. This suggests possible blood clots in your lungs.
- Seek emergency care if you’ve had previous heart problems and your chest pain feels similar to your prior heart attack or angina but medications aren’t helping.
- Don’t try to diagnose yourself. Doctors prefer evaluating chest pain early rather than having you delay during a real emergency.
- While waiting for help, sit or lie down comfortably. If you normally take aspirin and are not allergic, chew one regular aspirin—it may help if you’re having a heart attack. Try to stay calm.
Heart-Related Chest Pain
Understanding how heart problems cause chest pain helps you recognize them.
- Heart attack pain typically feels like pressure, squeezing, or fullness in the center or left side of your chest. Many people describe it as an elephant sitting on their chest. The discomfort usually lasts more than a few minutes or goes away and comes back. It often spreads to your left arm, but can also go to your jaw, neck, back, or right arm.
- Additional symptoms include shortness of breath, cold sweats, nausea, and lightheadedness. Some people, particularly women, elderly patients, and diabetics, have “atypical” symptoms—mainly shortness of breath, unusual fatigue, or vague discomfort rather than classic chest pressure.
- Angina is similar but less severe. It occurs when your heart needs more oxygen than narrowed coronary arteries can deliver—typically during exertion, stress, or cold weather. The discomfort feels like pressure or tightness and usually resolves within minutes after resting. If you have known angina and take nitroglycerin, the medication typically relieves it quickly.
- Unstable angina means chest pain occurring at rest, lasting longer, or not responding to medications. This is dangerous because it suggests a heart attack might happen soon.
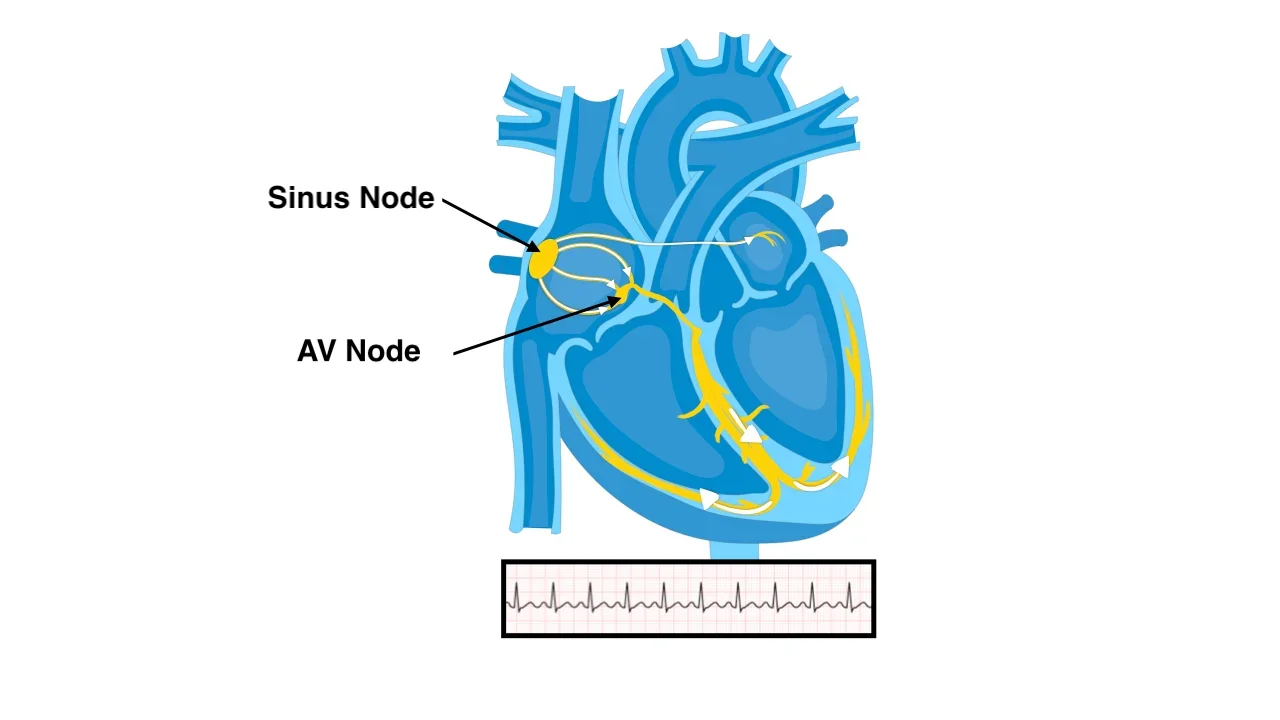
- Arrhythmias can cause chest discomfort. When your heart beats too fast—150-200 beats per minute or faster—you might feel chest tightness or pounding along with a racing heartbeat. This happens with conditions like atrial fibrillation, supraventricular tachycardia, or ventricular tachycardia. Very slow heart rates can also cause chest discomfort and lightheadedness.
- Aortic dissection causes sudden, severe, tearing or ripping pain in your chest or back. This is a medical emergency where the layers of your aorta separate. The pain is often described as the worst pain ever experienced.
- Pericarditis—inflammation of the sac surrounding your heart—causes sharp chest pain that worsens when lying down or taking deep breaths, and improves when sitting up and leaning forward.
Lung-Related Chest Pain
Lung problems cause different types of chest pain.
- Pulmonary embolism—blood clots in lung arteries—causes sharp chest pain that worsens with deep breathing. It comes with sudden shortness of breath, rapid heartbeat, and sometimes coughing up blood. Risk factors include recent surgery, long periods of immobility, cancer, or previous blood clots.
- Pneumonia causes chest pain that worsens with breathing or coughing. You typically have fever, cough producing colored mucus, and shortness of breath.
- Pleurisy—inflammation of the lung lining—causes sharp pain that worsens with breathing or coughing. You might hear yourself making a rubbing sound when breathing.
- Pneumothorax—a collapsed lung—causes sudden sharp chest pain and shortness of breath on one side. This can happen spontaneously, particularly in tall, thin young men, or after chest injuries.
Digestive Causes
Digestive problems frequently cause chest pain that can feel worryingly similar to heart problems.
- Heartburn or acid reflux causes burning pain behind your breastbone. It often occurs after eating, when lying down, or when bending over. You might taste acid in your mouth. Antacids usually provide relief.
- Esophageal spasm causes sudden, severe chest pain that can mimic heart attacks. Your esophagus—the tube from your throat to your stomach—contracts intensely. The pain can be severe and last from minutes to hours.
- Gallbladder problems cause pain in the upper right side of your chest or abdomen, often after eating fatty meals. The pain can spread to your back or right shoulder blade.
- Peptic ulcers cause burning pain in your upper abdomen or lower chest. The pain often improves with eating or taking antacids but returns hours later.
- Swallowing problems or esophagitis—inflammation of your esophagus—can cause pain behind your breastbone when swallowing.
Other Common Causes
Many non-dangerous conditions cause chest pain.
- Costochondritis—inflammation where ribs attach to breastbone—causes sharp pain that worsens with movement or pressing on the area. It’s tender to touch.
- Muscle strain from exercise, heavy lifting, or coughing causes pain that worsens with movement or breathing deeply. The muscles feel sore when pressed.
- Rib injuries from falls or impacts cause localized pain that worsens with breathing, coughing, or pressing on the area.
- Panic attacks cause chest tightness or pain along with rapid heartbeat, shortness of breath, sweating, shaking, and overwhelming fear. These symptoms can be identical to heart attacks, making them frightening. The key difference is panic attacks typically peak within 10 minutes and improve afterward.
- Shingles causes burning pain in a band on one side of your chest before the characteristic rash appears. The pain follows nerve pathways and stays on one side.
Getting Diagnosed
When you see a doctor for chest pain, they work to determine the cause through questions, examination, and tests.
- Your doctor asks detailed questions: Where exactly is the pain? What does it feel like—pressure, stabbing, burning, aching? When did it start? What makes it better or worse? What other symptoms do you have?
- Physical examination includes listening to your heart and lungs, pressing on your chest to see if that reproduces the pain, checking your blood pressure, and looking for other clues.
- An electrocardiogram records your heart’s electrical activity and can show whether you’re having or recently had a heart attack. This simple test takes just a few minutes.
- Blood tests check for enzymes released when heart muscle is damaged. Elevated troponin levels indicate heart damage. Other tests check for inflammation or blood clots.
- Chest X-rays look for lung problems, pneumonia, collapsed lungs, or heart enlargement.
- If heart problems are suspected, you might need a stress test—exercising on a treadmill while your heart is monitored—or coronary angiography to visualize your coronary arteries.
- CT scans can check for blood clots in lungs, aortic dissection, or other structural problems.
- Echocardiography uses ultrasound to visualize your heart’s structure and function.
- Upper endoscopy involves passing a flexible tube down your throat to examine your esophagus and stomach if digestive causes are suspected.
- Sometimes the cause isn’t immediately clear and requires time, observation, and multiple tests.
Treatment
Treatment depends entirely on what’s causing your chest pain.
- Heart attacks require immediate treatment to restore blood flow—usually emergency angioplasty with stenting. Medications include aspirin, blood thinners, and drugs to reduce heart workload.
- Angina is managed with medications that improve blood flow and reduce heart workload—nitroglycerin for quick relief, beta-blockers, calcium channel blockers, and long-acting nitrates for prevention. Severe cases need angioplasty or bypass surgery.
Arrhythmias need specific treatments depending on the type. Fast heart rates might respond to medications that slow the rhythm, or sometimes require procedures like electrical cardioversion—where a controlled shock resets your heart rhythm—or catheter ablation to fix the problem permanently. Very slow heart rates sometimes need pacemakers.
- Blood clots in lungs require blood thinners, initially in the hospital.
- Pneumonia needs antibiotics and supportive care.
- Heartburn responds to antacids and medications that reduce stomach acid production—proton pump inhibitors or H2 blockers. Lifestyle changes include avoiding trigger foods, not eating before bed, and elevating the head of your bed.
- Costochondritis and muscle strain improve with rest, ice, anti-inflammatory medications like ibuprofen, and avoiding activities that worsen pain.
- Panic attacks benefit from reassurance, breathing techniques, and sometimes medications or therapy to address underlying anxiety.
- Gallbladder problems often require surgery to remove the gallbladder if stones are causing repeated symptoms.
Key Points
- Chest pain has many causes ranging from life-threatening heart attacks to harmless muscle strain. Understanding different types helps you know when to seek emergency care.
- Call emergency immediately for chest pain that feels like pressure or squeezing lasting more than a few minutes, especially if it spreads to your arms, neck, or jaw, or comes with shortness of breath, sweating, or nausea.
- Heart attack pain typically feels like pressure or fullness in the center of your chest. Angina is similar but milder and occurs with exertion. Both need medical evaluation.
- Lung-related causes include blood clots, pneumonia, or collapsed lungs. These cause sharp pain that worsens with breathing.
- Digestive causes like heartburn are common and can mimic heart problems. The pain is often burning, occurs after eating, and improves with antacids.
- Musculoskeletal causes include costochondritis, muscle strain, or rib injuries. This pain worsens with movement or pressing on the area.
- Panic attacks cause chest tightness with rapid heartbeat, shortness of breath, and intense fear. Symptoms can feel identical to heart attacks.
- Diagnosis involves detailed questions, physical examination, electrocardiogram, blood tests, and sometimes imaging studies or stress tests.
- Treatment depends on the cause. Heart problems need medications and sometimes procedures. Digestive problems respond to antacids and lifestyle changes. Musculoskeletal pain improves with rest and anti-inflammatory medications.
- Don’t ignore chest pain or try to diagnose yourself. When in doubt, seek medical attention. It’s better to have harmless chest pain evaluated than to delay during a real emergency.
Reference: Chest Pain