Bradycardia is a condition in which the heart beats more slowly than normal. In adults, a resting heart rate below 60 beats per minute is generally considered bradycardia. For some people, a slow heart rate is completely normal and even a sign of good physical fitness. For others, it may reflect a problem with the heart’s electrical system that requires evaluation.
The key to understanding bradycardia is recognizing that a low heart rate is not automatically dangerous. What matters most is why the heart rate is slow and how the body responds to it.
How Heart Rate Is Normally Regulated
The heart’s rhythm is controlled by its electrical system, which adjusts the heart rate based on the body’s needs. During sleep or deep relaxation, the heart naturally slows down. During physical activity or stress, it speeds up to deliver more oxygen-rich blood.
Bradycardia becomes a concern when the heart cannot increase its rate appropriately or when the slow rhythm leads to symptoms caused by reduced blood flow to the brain and other organs.
When a Slow Heart Rate Is Normal
A low resting heart rate can be entirely normal in certain situations. Well-trained athletes often have slow heart rates because their hearts pump blood more efficiently with each beat. During sleep, heart rate commonly drops without causing any harm.
In these cases, the electrical system is functioning properly, and the slow rate reflects normal physiological adaptation rather than disease.
Symptoms of Bradycardia
Many people with mild bradycardia have no symptoms at all. Symptoms tend to occur when the heart rate becomes too slow to meet the body’s demands.
Before listing symptoms, it is important to note that symptoms—not the heart rate number alone—often determine whether treatment is needed.
Common symptoms include:
- Fatigue or low energy
- Dizziness or lightheadedness
- Shortness of breath during activity
- Exercise intolerance
- Confusion or difficulty concentrating
- Fainting or near-fainting
When symptoms are present, bradycardia should be evaluated promptly.
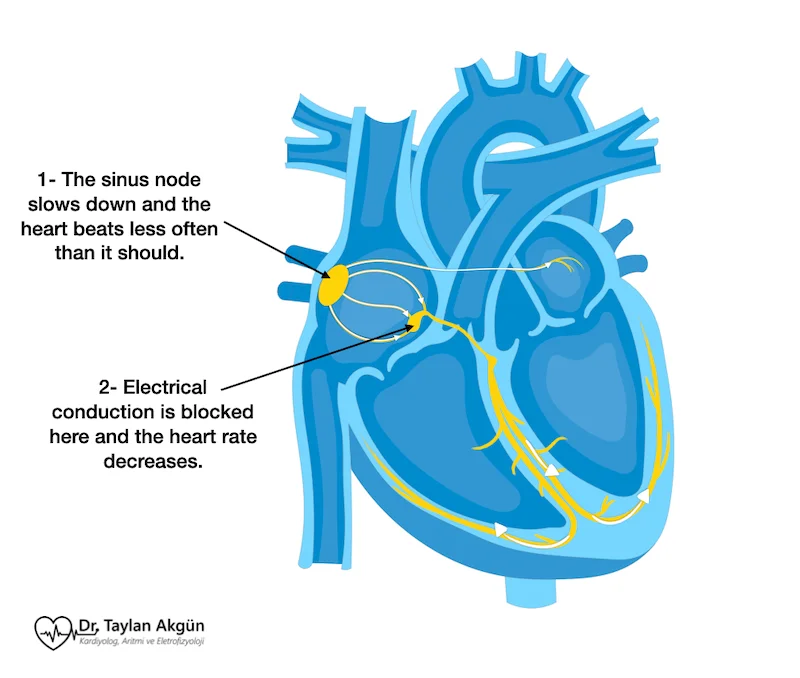
Why Bradycardia Occurs
Bradycardia can result from problems in the heart’s natural pacemaker or in the pathways that carry electrical signals through the heart. Age-related changes in the electrical system are a common cause.
Other contributing factors include:
- Heart Block, where electrical signals are delayed or blocked
- Certain medications, such as beta blockers or calcium channel blockers
- Hypothyroidism
- Electrolyte imbalances
- Inflammation or scarring of heart tissue
In some individuals, bradycardia is present from birth, while in others it develops gradually over time.
Types of Bradycardia
Bradycardia can take several forms, depending on where the electrical slowdown occurs.
- Sinus bradycardia originates from the heart’s natural pacemaker and may be normal or abnormal depending on symptoms and context.
- Conduction-related bradycardia occurs when electrical signals fail to reach the ventricles reliably, as seen in advanced forms of heart block. These forms are more likely to cause symptoms and require treatment.
How Bradycardia Is Diagnosed
Diagnosis begins with documenting the heart rhythm, usually with an electrocardiogram. Because bradycardia may be intermittent, longer-term rhythm monitoring is often needed.
Additional tests may be used to evaluate heart structure, assess exercise response, and identify reversible causes such as thyroid dysfunction or medication effects.
The goal of testing is to determine whether the slow heart rate is benign or clinically significant.
Treatment Options for Bradycardia
Treatment depends on the cause and the presence of symptoms. Many people with asymptomatic bradycardia require no treatment beyond observation and regular follow-up.
If medications are contributing to a slow heart rate, adjusting or discontinuing them may resolve the problem. Treating underlying conditions such as hypothyroidism or electrolyte imbalance can also restore a normal rhythm.
When bradycardia causes significant symptoms or results from advanced conduction disease, implantation of a Pacemaker may be recommended. A pacemaker provides reliable electrical stimulation to maintain an appropriate heart rate and prevent pauses that can lead to dizziness or fainting.
Pacemaker therapy does not cure the underlying electrical disorder, but it effectively restores a safe and stable heart rhythm.
Living With Bradycardia
Living with bradycardia depends largely on its cause. Many people live normal, active lives with no limitations. For those who require treatment, modern therapies are highly effective and allow excellent quality of life.
Understanding the condition, recognizing symptoms, and maintaining regular medical follow-up are essential parts of long-term management.
Can Bradycardia Be Treated With Ablation?
In most patients, bradycardia is not treated with ablation. However, in selected situations, catheter-based procedures may play a role.
In some individuals, frequent premature beats originating from the atria can suppress the normal heart rhythm and lead to a slow average heart rate or symptoms resembling bradycardia. In these cases, catheter ablation targeting the premature beats can restore a more stable and appropriate heart rate.
In addition, patients with reflex (vasovagal) syncope often have low resting heart rates due to excessive vagal activity. In carefully selected patients with recurrent symptoms, cardioneuroablation—a procedure that modifies specific cardiac nerve pathways—may reduce this excessive reflex and lead to an increase in resting heart rate, potentially avoiding the need for pacemaker therapy.
In Summary
Bradycardia refers to a slower-than-normal heart rate. While it can be a normal finding in healthy individuals, it may also reflect a problem with the heart’s electrical system. Determining the cause and assessing symptoms are crucial. With proper evaluation and individualized treatment, most people with bradycardia can be managed safely and effectively.
Reference: Bradycardia