What is a cardiac pacemaker?
A cardiac pacemaker is a small medical device that regulates your heart rhythm. When your heart beats too slowly, pauses, or works irregularly, the pacemaker activates, sends electrical impulses to the heart, and restores a normal rhythm.
The device is placed in the upper part of the chest, usually on the left side beneath the collarbone. Through thin wires, it delivers electrical signals to the heart and regulates your heartbeats.
A cardiac pacemaker continuously monitors your heart rhythm. If your heart rate is normal, the device remains on standby. When your heart rate falls below a certain level or when a heartbeat is absent, the device becomes active.
The pacemaker sends small electrical impulses to the heart to trigger contraction. These impulses are very mild and are not felt.
Why is a cardiac pacemaker implanted?
There are many reasons why a cardiac pacemaker may be needed.
Bradycardia (Slow heart rate)
When the heart beats slower than normal, this is called bradycardia. A resting heart rate below 60 beats per minute is considered slow. In some people this can be normal, but if it causes symptoms, treatment is required.
Bradycardia can cause dizziness, fatigue, shortness of breath, and fainting. A cardiac pacemaker keeps the heart rate at a normal level and relieves these symptoms.
Heart block
Heart block occurs when there is a problem with the transmission of electrical signals in the heart. Signals cannot be properly conducted from the upper chambers to the lower chambers. This can lead to slow heartbeats or pauses.
Complete heart block can be life-threatening and usually requires a cardiac pacemaker.
Sinus node dysfunction
The sinus node is the heart’s natural pacemaker. It tells the heart when to beat. When the sinus node does not function properly, the heart may beat too slowly, pause, or alternate between fast and slow rhythms.
This condition is also called sick sinus syndrome and often requires a cardiac pacemaker.
Atrial fibrillation treatment
In some patients with atrial fibrillation, a cardiac pacemaker may be used to control the heart rate. A pacemaker may be needed when adequate control cannot be achieved with medications or when rate-slowing drugs cause the heart to beat too slowly.
Heart failure
In some patients with heart failure, a special type of cardiac pacemaker is used. This device is called a cardiac resynchronization therapy (CRT) device. It improves pumping efficiency by synchronizing the contractions of both sides of the heart.
How is a cardiac pacemaker implanted?
A cardiac pacemaker is usually implanted in a hospital electrophysiology laboratory under local anesthesia, where only the area where the device will be placed is numbed. General anesthesia is not required in most patients.
A small incision is made in the upper left part of the chest. Thin wires are advanced through the veins and positioned in the appropriate locations within the heart.
After the wires are tested, the pacemaker device is placed under the chest muscle and the incision is closed. The procedure usually takes about one hour. You may be discharged the same day or the following day.
Mild pain and discomfort in the first few days after the procedure are normal. Most people achieve full recovery within 4–6 weeks.
Types of cardiac pacemakers
Single-chamber cardiac pacemaker: The simplest type. It uses one wire connected to either the right atrium or the right ventricle. It is commonly used for the treatment of bradycardia.
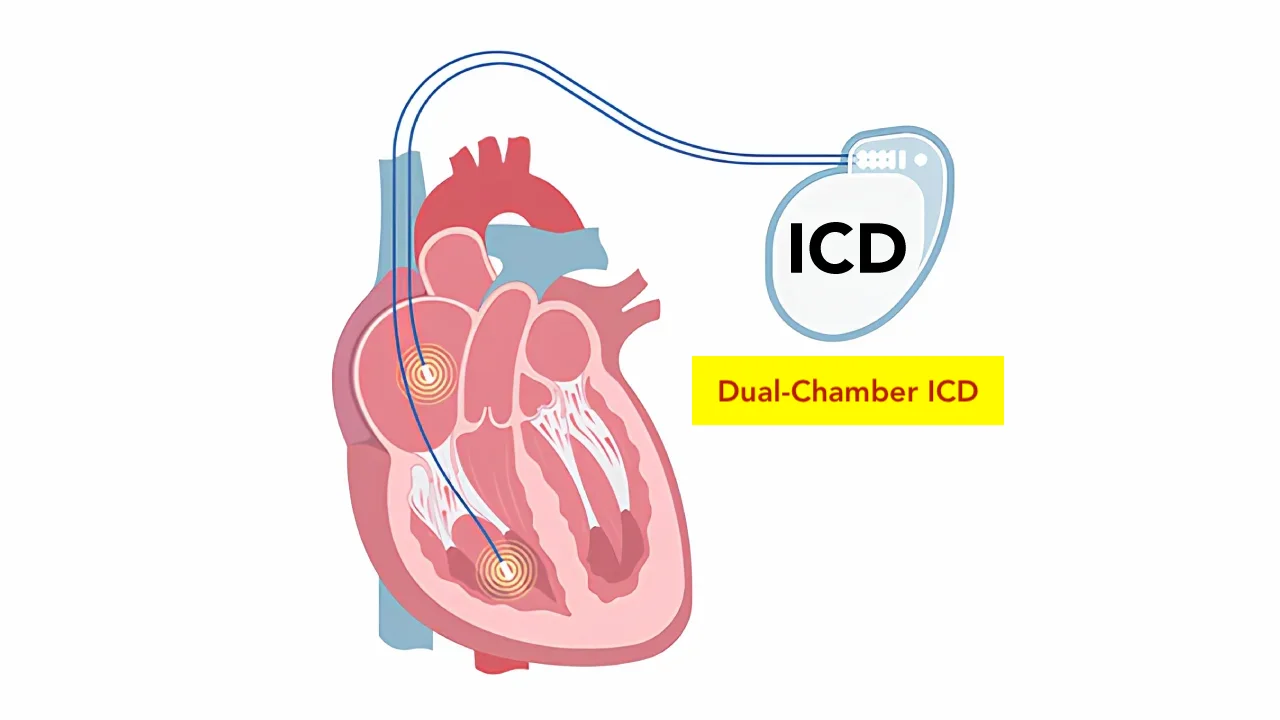
Dual-chamber cardiac pacemaker: Uses two wires—one placed in the right atrium and the other in the right ventricle. It monitors and regulates both atrial and ventricular activity. It provides more physiological pacing and is the most commonly used type.
Three-chamber cardiac pacemaker (CRT): Used in the treatment of heart failure. It has three wires that stimulate the right atrium, right ventricle, and left ventricle, allowing synchronized contraction of both sides of the heart.
Leadless cardiac pacemaker: A newer generation of very small pacemakers. They are implanted directly inside the heart and do not require wires.
What happens if a cardiac pacemaker is not implanted?
If your heart rate is very slow or pauses occur, your body and brain may not receive enough blood. This can lead to persistent fatigue, dizziness, and difficulty concentrating. Daily activities may become difficult, and quality of life can significantly decline.
You may experience recurrent fainting episodes. Falls during fainting can result in serious injuries, including head trauma, bone fractures, or internal bleeding.
The most serious risk is sudden cardiac arrest. The heart may stop completely, which is a life-threatening condition. The risk of sudden cardiac arrest is particularly high in conditions such as complete heart block.
When implantation of a cardiac pacemaker is recommended, it represents a serious medical necessity. Your doctor will discuss the risks and benefits with you. If you have concerns, you should discuss them with your doctor, but unnecessary delays can be life-threatening.
What are the benefits of a cardiac pacemaker?
A cardiac pacemaker provides many benefits:
- Fainting and dizziness are eliminated
- Fatigue decreases and energy levels improve
- Shortness of breath improves
- Exercise capacity increases
- Quality of life improves significantly
- Risk of sudden cardiac arrest decreases
- In some cases, life expectancy increases
Most patients experience marked improvement in symptoms after pacemaker implantation and can lead a more active life.
Is cardiac pacemaker implantation risky?
Like any medical procedure, cardiac pacemaker implantation carries some risks, but it is generally a safe procedure.
- Bleeding or bruising
- Infection
- Blood vessel injury
- Air leakage into the lung (pneumothorax)
- Fluid accumulation around the heart
- Temporary arrhythmias during lead placement
- Lead fracture or displacement
- Allergic reactions
Most of these complications are rare, and the risk is very low in experienced centers. Regular follow-up allows early detection and treatment of potential problems.
FAQs about cardiac pacemakers
Living with a cardiac pacemaker
You can live a normal life with a cardiac pacemaker. Most daily activities can be performed safely.
During the first 4–6 weeks, some restrictions apply. You should not raise the arm on the side of the pacemaker above shoulder level or lift heavy objects. These restrictions are lifted after this period.
Everyday electronic devices such as mobile phones, computers, televisions, and microwave ovens do not affect your cardiac pacemaker. You should inform security personnel about your pacemaker at airport security checkpoints.
Some industrial equipment and strong magnetic fields may interfere with the device. You should avoid close proximity to power plants, strong magnets, and welding machines.
You can exercise, swim, and travel. Contact sports should be avoided, as a direct blow to the chest may damage the device.
How is a cardiac pacemaker checked?
Your cardiac pacemaker must be checked regularly. The first check is usually performed 2–4 weeks after implantation. Thereafter, follow-ups are recommended every 3–6 months.
During follow-up, your doctor will:
- Check battery life
- Assess lead function
- Optimize device settings
- Monitor your heart rhythm
- Adjust programming if necessary
The lifespan of a cardiac pacemaker battery is usually between 5 and 15 years. As the battery approaches depletion, follow-ups become more frequent. When the battery is depleted, only the device is replaced with a minor procedure; the leads usually remain in place.
Some newer cardiac pacemakers can be monitored remotely. Data can be transmitted to your doctor from home. However, regular in-person follow-ups remain important.
When to see a doctor?
Contact your doctor immediately if you experience:
- Dizziness or fainting
- Palpitations or irregular heartbeats
- Shortness of breath
- Chest pain
- Persistent hiccups
- Muscle twitching
- Redness, swelling, or discharge at the incision site
- Protrusion or movement of the device
These symptoms require medical evaluation.
What is a cardiac pacemaker card?
You will be given a cardiac pacemaker identification card. Always carry this card with you. It contains information about the brand, model, implantation date, and your doctor’s details.
This card is important in emergencies, airport security checks, and during medical procedures.
You can read more about what to consider after cardiac pacemaker implantation and cardiac pacemaker replacement at the links below.
References: Pacemaker