Epicardial ablation is a specialized treatment for arrhythmias that start on the outer surface of the heart. It is used when standard treatments are not effective. When carefully planned and performed by experienced specialists, it can safely restore heart rhythm control and significantly improve your quality of life.
Why Epicardial Ablation Is Sometimes Needed
In many people, arrhythmias can be treated successfully from inside the heart. But sometimes, the abnormal electrical signals are located mainly on the outside of the heart muscle.
When this happens, treating the problem from inside may not fully reach the affected area. This means the rhythm problem can continue despite treatment.
Epicardial ablation allows doctors to treat the rhythm problem directly at its source, which can greatly improve the chances of long-term success.
Conditions Commonly Treated With Epicardial Ablation
Epicardial ablation is most often used to treat serious rhythm problems that start in the lower chambers of the heart, called ventricular arrhythmias.
You may be advised to have this procedure if your rhythm problem is related to:
- Scar tissue from previous heart disease
- Certain inherited heart conditions
- Inflammation of the heart muscle
This includes conditions such as:
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
- Brugada Syndrome
- Rhythm problems after myocarditis
- Some types of heart muscle disease
Your doctor will decide if epicardial ablation is right for you based on your symptoms, test results, heart scans, and previous treatments.
How Epicardial Ablation Works
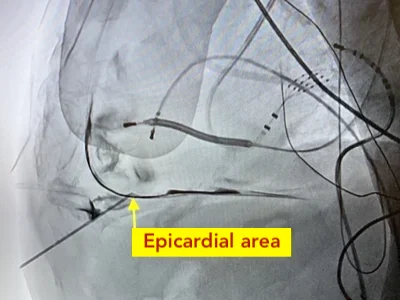
Epicardial ablation is performed by carefully reaching the space around your heart, called the pericardial space.
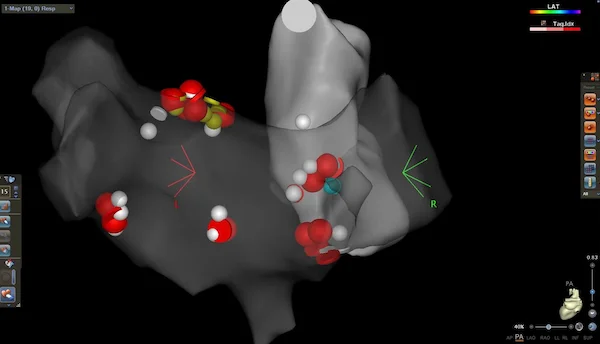
Through this space, thin flexible tubes (catheters) are gently guided to the outer surface of your heart. These catheters allow doctors to record electrical signals and find the exact area causing your rhythm problem.
Once the problem area is found, controlled energy is applied to stop the abnormal electrical signals and restore a normal heart rhythm.
The Epicardial Ablation Procedure
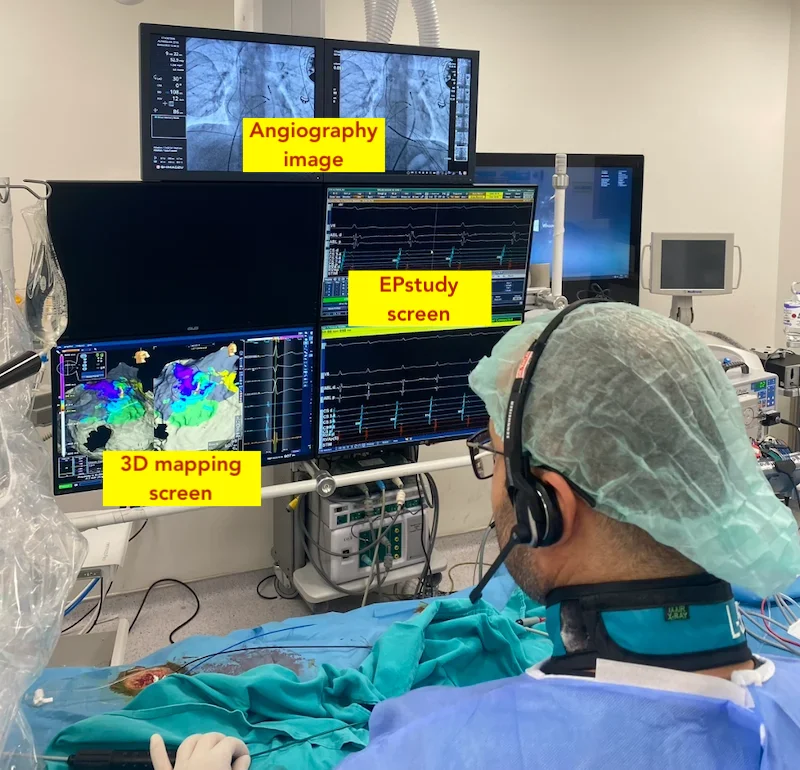
Epicardial ablation is performed in a specialized heart rhythm laboratory by experienced teams.
During the procedure:
- You will receive local anesthesia and medication to help you relax, or general anesthesia if needed
- A small needle is used to safely reach the space around your heart, usually just below the breastbone
- Thin catheters are guided to your heart
- The problem area is carefully mapped and treated
- Your heart rhythm and vital signs are monitored continuously
In many cases, treatment from inside and outside the heart is done during the same session to improve success.
The procedure usually takes several hours, depending on complexity.
Recovery After Epicardial Ablation
After the procedure, you will stay in the hospital for one to several days so your heart rhythm and recovery can be closely monitored.
You may feel mild chest discomfort or soreness, which is common and usually improves with simple pain relief medication.
During recovery:
- You should avoid heavy activity for a short period
- You can gradually return to normal daily activities as advised by your doctor
- Follow-up visits help ensure proper healing and rhythm control
Most people recover well and return to daily life within a short time.
Benefits of Epicardial Ablation
If this treatment is right for you, epicardial ablation can:
- Reduce or stop dangerous heart rhythm episodes
- Improve symptoms such as palpitations, dizziness, and fainting
- Reduce the need for long-term medication
- Lower the number of shocks in people with implanted defibrillators
- Improve your overall quality of life
For some people, this procedure offers the best chance of long-lasting rhythm control.
Risks and Safety
Epicardial ablation is a complex procedure and carries some risks. Because the treatment is performed close to important organs and blood vessels, careful planning and expert technique are essential.
Your medical team will carefully explain the possible risks and benefits before the procedure. Advanced imaging and continuous monitoring help keep complications to a minimum.
When performed in experienced centers, epicardial ablation is generally safe.
Living After Epicardial Ablation
After treatment, regular follow-up is important to check your heart rhythm and overall heart health.
You may need heart rhythm monitoring, medication adjustments, and occasional scans. Improvement may happen quickly or gradually, depending on your condition.
Most people notice significant symptom relief and are able to return to a more active and comfortable daily life.