Cardioneuroablation (CNA) is a specialized catheter-based procedure used to treat certain conditions caused by excessive vagal (parasympathetic) influence on the heart. It is most commonly considered in patients with recurrent reflex (vasovagal) syncope or severe functional bradycardia, where episodes of fainting or marked heart rate slowing occur despite lifestyle measures and medical therapy.
The goal of cardioneuroablation is not to treat a traditional arrhythmia, but to modify abnormal nerve signals that excessively slow the heart or interrupt normal electrical conduction.
Why Cardioneuroablation Is Performed
In some individuals, the autonomic nervous system overreacts to certain triggers such as prolonged standing, emotional stress, pain, or sudden changes in posture. This exaggerated reflex can cause a sudden drop in heart rate, blood pressure, or both, leading to dizziness or fainting.
When these episodes are frequent, unpredictable, or associated with injury—and do not respond adequately to conservative treatment—cardioneuroablation may be considered as an alternative to long-term medication or pacemaker implantation in selected patients.
How Cardioneuroablation Works
The heart is influenced by small nerve clusters called cardiac ganglionated plexi, which are part of the autonomic nervous system. In susceptible patients, these nerve pathways can trigger excessive slowing of the heart.
During cardioneuroablation, targeted energy is delivered to specific areas of the heart that contain these nerve clusters. By reducing abnormal vagal input, the procedure aims to normalize heart rate control and prevent reflex-related pauses or extreme slowing.
This treatment does not eliminate normal autonomic function; rather, it reduces the exaggerated reflex response that causes symptoms.
Who May Be a Candidate for Cardioneuroablation?
Cardioneuroablation may be considered in patients with:
- Recurrent reflex (vasovagal) syncope with documented cardioinhibitory responses
- Symptomatic functional bradycardia not caused by structural conduction disease
- Recurrent pauses related to excessive vagal tone
- Syncope where pacemaker implantation is being considered but may be avoidable
Careful evaluation is essential to ensure that symptoms are due to functional autonomic mechanisms rather than irreversible conduction system disease.
What Happens During the Procedure?
Cardioneuroablation is performed in a specialized electrophysiology laboratory. Sedation is typically used so the patient is comfortable and relaxed.
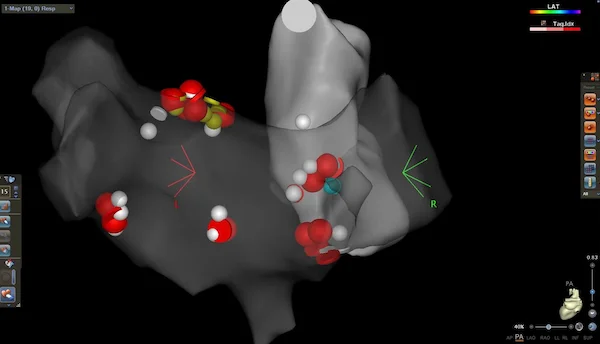
Catheters are guided to the heart through blood vessels, usually from the groin. Using advanced electrical mapping and physiological testing, the areas responsible for excessive vagal influence are identified. Controlled ablation energy is then delivered to these targets.
The procedure duration varies but is comparable to other catheter ablation procedures.
What Will I Feel During and After the Procedure?
Most patients do not feel pain during the procedure due to sedation. Afterward, temporary fatigue or mild chest discomfort may occur.
Many patients notice improvement in symptoms relatively early, with fewer fainting episodes and more stable heart rates. Follow-up monitoring is important to assess response.
Recovery and Follow-Up
Recovery after cardioneuroablation is generally quick. Most patients return home within one or two days and resume normal activities shortly thereafter.
Follow-up focuses on symptom monitoring, heart rhythm assessment, and long-term evaluation of syncope recurrence.
Risks and Considerations
Cardioneuroablation is performed in selected centers with expertise in autonomic modulation. As with any invasive procedure, risks exist, but serious complications are uncommon when performed by experienced teams.
Because this is a relatively newer treatment strategy, careful patient selection and long-term follow-up are essential.
In Summary
Cardioneuroablation is a catheter-based treatment designed to reduce excessive vagal influence on the heart in patients with recurrent reflex syncope or functional bradycardia. By targeting specific autonomic nerve pathways, it can stabilize heart rate control and reduce fainting episodes without the need for permanent pacing in selected individuals. When appropriately chosen, cardioneuroablation offers a promising and patient-centered treatment option for autonomic-related heart rhythm disorders.
Reference: Cardioneuroablation for Treating Vasovagal Syncope