Atrial fibrillation (AFib or AF) is a common heart rhythm disorder in which the heart loses its regular pattern and begins to beat in an irregular and often unpredictable way. Some people notice it immediately as a strong or uncomfortable sensation in the chest, while others may live with it for years without realizing anything is wrong.
What makes atrial fibrillation especially important is not only how it feels, but what it can quietly cause over time. Even when symptoms are mild—or completely absent—it can increase the risk of stroke, heart failure, and long-term weakening of the heart muscle. For this reason, atrial fibrillation is not just a rhythm issue, but a condition that requires careful evaluation and follow-up.
How Atrial Fibrillation Affects the Heart
In a healthy heart, each heartbeat follows a clear sequence. The electrical signal starts at a natural control center and spreads smoothly, allowing the heart chambers to contract in an organized and efficient way. This coordination ensures that blood moves forward with every beat.
In atrial fibrillation, this order is disrupted. Instead of one clear signal, many small and chaotic signals occur at the same time in the upper chambers of the heart. As a result, these chambers do not contract effectively. The heartbeat becomes irregular, and blood flow inside the heart slows down, especially in certain areas where blood can stagnate.
This change in flow is the key reason atrial fibrillation carries risks beyond palpitations or discomfort.
Symptoms of Atrial Fibrillation
The way atrial fibrillation feels can vary greatly from person to person. Some people experience clear and disturbing symptoms, while others may feel almost nothing. In many cases, symptoms develop gradually and are initially attributed to stress, aging, or lack of fitness.
Before listing common symptoms, it is important to understand that symptoms are not a reliable measure of risk. A person with few or no symptoms can still face serious complications.
Common symptoms include:
- A sensation of irregular or fast heartbeat
- Shortness of breath, especially during exertion
- Easy fatigue or reduced exercise capacity
- Dizziness or lightheadedness
- Chest discomfort or pressure
- A general feeling of weakness or lack of energy
In older adults, atrial fibrillation may present more subtly, sometimes only as reduced stamina, confusion, or frequent falls.
Why Atrial Fibrillation Develops
Atrial fibrillation usually does not have a single cause. Instead, it develops when the structure or electrical properties of the heart change over time. These changes make the atria more vulnerable to chaotic electrical activity.
Many conditions can contribute to this process. The most common include:
- High blood pressure, which gradually enlarges and stiffens the atria
- Heart valve disease or previous heart surgery
- Coronary artery disease or heart failure
- Obesity and obstructive sleep apnea
- Thyroid disorders, especially an overactive thyroid
- Excessive or long-term alcohol consumption
- Aging, which naturally alters heart tissue
Often, several of these factors are present at the same time. Identifying and managing them is an essential part of treatment.
How Atrial Fibrillation Is Diagnosed
The diagnosis of atrial fibrillation is usually straightforward once the rhythm is documented. However, because atrial fibrillation can come and go, it may not always be captured during a short medical visit.
Diagnosis typically begins with an electrocardiogram, a simple test that records the heart’s electrical activity. When atrial fibrillation is present, the rhythm appears irregular and lacks the normal repeating pattern seen in a healthy heartbeat.
If atrial fibrillation is suspected but not immediately recorded, longer monitoring may be used. Ultrasound imaging of the heart helps assess heart size, pumping function, and valve structure, while blood tests may reveal conditions that contribute to the rhythm disturbance.
Why Stroke Risk Is Central in Atrial Fibrillation
One of the most serious consequences of atrial fibrillation is stroke. When the atria do not contract effectively, blood can pool in certain parts of the heart instead of flowing freely. Over time, this pooled blood can form clots.
If a clot breaks loose and travels to the brain, it can block a blood vessel and cause a stroke. This risk exists even when atrial fibrillation causes little or no discomfort. For this reason, preventing stroke is often the first priority in treatment.
Treatment Goals in Atrial Fibrillation
Treatment of atrial fibrillation is individualized, but it generally focuses on three main goals: reducing stroke risk, controlling the heart rate, and restoring or maintaining a more normal rhythm when appropriate.
Medications and Heart Rate Control
In many patients, medications are used to slow the heart rate and make the rhythm more tolerable. These drugs do not necessarily stop atrial fibrillation itself, but they help the heart work more efficiently and reduce symptoms such as shortness of breath or fatigue.
Other medications may be prescribed to reduce the risk of blood clots. These blood-thinning treatments do not correct the rhythm, but they play a critical role in preventing stroke.
Rhythm Control and Catheter Ablation
For some patients, especially those with ongoing symptoms or reduced quality of life, restoring a normal rhythm becomes an important goal. This can be attempted with medications or procedures designed to reset or stabilize the heart’s electrical activity.
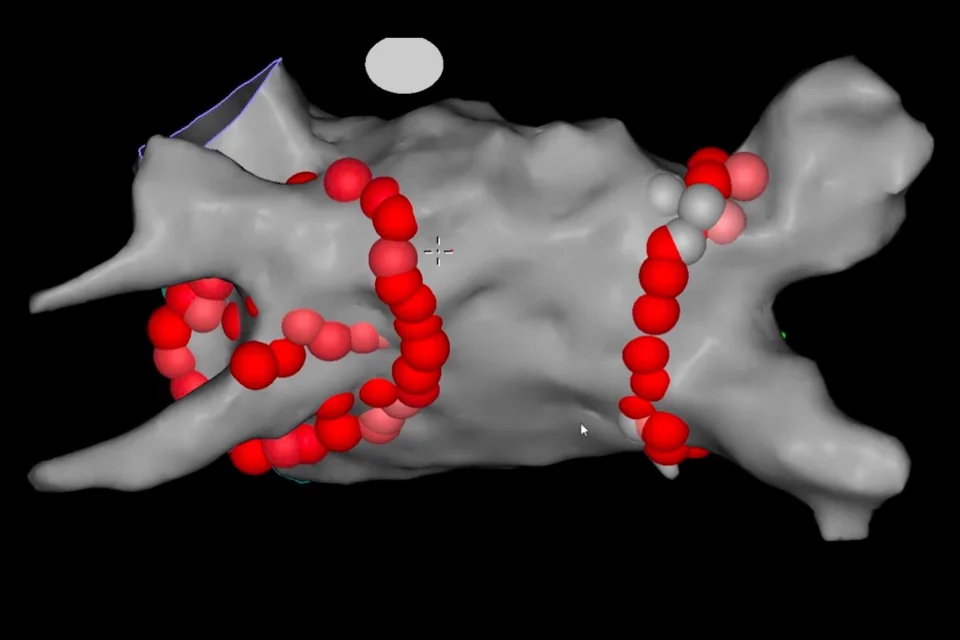
One commonly used procedure is catheter ablation. During this procedure, thin tubes are guided through blood vessels to the heart. The areas responsible for triggering abnormal electrical signals are carefully identified and treated to prevent these signals from spreading. Over time, this can reduce or eliminate episodes of atrial fibrillation.
Ablation is not a cosmetic or minor intervention. It is a structured treatment aimed at correcting the underlying electrical problem and is recommended only after careful evaluation.
Left Atrial Appendage Closure: What It Really Means
In some patients, long-term use of blood-thinning medication is not possible due to bleeding risk or other medical concerns. In these cases, an alternative approach may be considered.
Inside the left atrium, there is a small pouch where blood clots commonly form during atrial fibrillation. Left atrial appendage closure is a procedure designed to seal off this area so that blood can no longer collect there.
This is done by placing a specially designed device inside the heart through a catheter-based procedure. Once in place, the device permanently blocks the pouch, reducing the risk of clot formation. Over time, heart tissue grows over the device, making it part of the heart’s structure.
This procedure does not treat atrial fibrillation itself, but it addresses one of its most dangerous consequences.
Cardioversion: Restoring the Heart’s Rhythm
In some patients, atrial fibrillation does not stop on its own and continues despite medication. In these situations, restoring the heart’s normal rhythm may be considered through a procedure called cardioversion.
Cardioversion is a controlled medical procedure designed to reset the heart’s rhythm. It can be performed using medication or a brief, carefully delivered electrical shock. Although the word “shock” can sound alarming, the procedure is done under short-acting anesthesia, so the patient does not feel pain or discomfort.
Before cardioversion, doctors carefully evaluate the risk of blood clots. If atrial fibrillation has been present for more than a short period, blood-thinning treatment is usually required beforehand to reduce the risk of stroke. In some cases, imaging is used to make sure no clots are present inside the heart.
Cardioversion does not cure atrial fibrillation permanently. Instead, it gives the heart a chance to return to a normal rhythm. In many patients, additional treatments are needed afterward to help maintain that rhythm and prevent recurrence.
Treating the Underlying Causes
Atrial fibrillation rarely exists in isolation. In most patients, it develops as a consequence of other medical conditions that place stress on the heart over time. Treating atrial fibrillation without addressing these underlying problems is often ineffective.
High blood pressure is one of the most important contributors and must be carefully controlled. Excess body weight increases strain on the heart and promotes inflammation, making rhythm disturbances more likely. Sleep apnea, when left untreated, repeatedly stresses the heart during the night and strongly promotes atrial fibrillation. Thyroid disorders, particularly an overactive thyroid, can directly trigger abnormal rhythms.
Heart valve disease, coronary artery disease, and heart failure also play a major role. When these conditions are treated appropriately, atrial fibrillation becomes easier to control and may occur less frequently.
For this reason, successful management of atrial fibrillation is not limited to rhythm-focused treatments alone. It requires a comprehensive approach that targets the heart as well as the conditions that affect it.
Where These Fit in the Overall Treatment Strategy
Cardioversion, catheter ablation, medications, and stroke prevention strategies are not competing options. They are complementary tools used at different stages and for different purposes. Equally important is the correction of the conditions that allowed atrial fibrillation to develop in the first place.
When rhythm control strategies are combined with treatment of underlying diseases and lifestyle modifications, long-term outcomes improve significantly.
Preventing Progression and Recurrence
While not all cases of atrial fibrillation can be prevented, lifestyle changes play a powerful role in slowing progression and reducing recurrence. Maintaining a healthy weight, managing blood pressure, treating sleep apnea, limiting alcohol intake, and staying physically active all contribute to better rhythm control.
These measures are not optional extras; they are an essential part of long-term management.
Living With Atrial Fibrillation
Atrial fibrillation is often a long-term condition, but it does not have to define daily life. With appropriate treatment, regular follow-up, and attention to contributing factors, many people live active and fulfilling lives.
Understanding the condition is the first step toward managing it effectively. A well-informed patient is better equipped to make decisions, recognize changes, and participate actively in treatment.
In Summary
Atrial fibrillation is more than an irregular heartbeat. It is a condition that affects how the heart works and how blood flows through the body. While it may be silent at times, its consequences can be serious if left unaddressed. Comprehensive care—focused on stroke prevention, symptom control, and long-term heart health—allows most patients to manage atrial fibrillation safely and confidently.
Reference: Atrial Fibrillation