Brugada Syndrome affects your heart’s electrical activity. Each beat of your heart occurs with electrical signals created by the passage of ions such as sodium and potassium through cell membranes. In Brugada Syndrome, there is a genetic defect in these ion channels, especially sodium channels. This defect disrupts the order of electrical signals, leading to a characteristic ECG pattern in your heart’s right lower chamber (right ventricle). This pattern can be triggered while at rest or by conditions such as fever.
- What is Brugada syndrome?
- What are the symptoms of Brugada syndrome?
- What causes Brugada syndrome?
- Who develops Brugada syndrome?
- How is Brugada syndrome diagnosed?
- How is Brugada syndrome treated?
- Nutrition in Brugada syndrome
- Exercise in Brugada syndrome
- What are the risks of Brugada syndrome?
- How can Brugada syndrome be prevented?
- When should you consult a doctor?
What is Brugada syndrome?
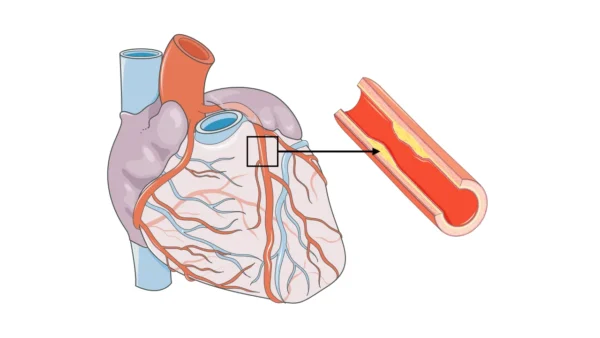
Brugada Syndrome is a rare, congenital disease that affects the electrical system in the lower chambers (ventricles) of your heart. Although your heart’s structure and muscle tissue are normal, an abnormal rhythm can occur due to dysfunction in the channels that carry electrical signals. This condition can occur especially at night or during rest, causing dangerous arrhythmias such as ventricular fibrillation. The seriousness of Brugada Syndrome is that it can lead to sudden death even without showing symptoms.
What are the symptoms of Brugada syndrome?
Brugada Syndrome is usually an insidious disease that does not show symptoms. Most of the time, it cannot be diagnosed until a patient experiences fainting or sudden cardiac arrest. Therefore, recognizing the symptoms of the syndrome is of great importance, especially for those with a family history of sudden death. The most common symptoms are fainting (syncope), abnormal heart rhythms (arrhythmia), and nighttime shortness of breath.
The main symptoms of Brugada Syndrome are:
- Fainting (Syncope): Occurs due to the brief stopping of blood flow to the brain during a dangerous arrhythmia. It usually develops suddenly without any warning.
- Palpitations: You may feel your heart beating fast and irregularly. This may be one of the arrhythmias caused by Brugada.
- Nighttime Shortness of Breath (Nocturnal Agonal Breathing): You may experience abnormal breathing patterns or shortness of breath during sleep. This condition may indicate an arrhythmia that starts during sleep.
- Sudden Death: This is the most feared symptom. It usually occurs without any warning in young and apparently healthy individuals.
What causes Brugada syndrome?
Brugada Syndrome is a completely genetic disease. It results from a mutation in genes responsible for the production of ion channels that direct your heart’s electrical signals. This genetic defect is usually inherited from mother or father, but sometimes it can also appear as a new mutation not previously seen in the family.
The main causes leading to Brugada Syndrome are:
- Genetic Mutation: The most common cause of Brugada Syndrome is mutations in the SCN5A gene that codes for the heart’s sodium channels. These mutations lead to disruptions in the heart’s electrical cycle.
- Family History: Individuals with a family history of Brugada Syndrome or unexplained sudden death have a higher risk of developing the syndrome.
There are also some factors that can trigger arrhythmias in Brugada Syndrome. These triggers do not cause the syndrome itself but can initiate attacks in a risky patient:
- High fever, especially in children and young people, can trigger dangerous arrhythmias.
- Some medications such as antidepressants or anti-arrhythmic drugs that affect the heart’s electrical system are risky.
- Excessive alcohol intake can trigger arrhythmias in people with Brugada Syndrome.
- High vagal tone, i.e., excessive activity of the nervous system that activates when the body is at rest, can cause arrhythmias during sleep.
Who develops Brugada syndrome?
Since Brugada Syndrome is a genetic disease, it can appear at any age, but it is often diagnosed in young adult men, especially between the ages of 30-40. It is 8-10 times more common in men than women. It is more commonly seen in Asian communities, especially in Japan, Thailand, and the Philippines.
How is Brugada syndrome diagnosed?
Brugada Syndrome diagnosis is usually made with an electrocardiogram (ECG) and clinical evaluation. The most important tool for diagnosis is the ECG, which shows your heart’s electrical activity. However, the characteristic pattern on ECG may not always be visible, so special tests may also be needed.
The main methods used in Brugada Syndrome diagnosis are:
- ECG: Records your heart’s electrical activity and shows the characteristic pattern called “coved-tip” specific to Brugada Syndrome. This pattern can become more pronounced at rest or with conditions such as fever.
- Drug Provocation Test: In people with suspicious findings on ECG or those with a family history of the syndrome, special drugs called sodium channel blockers are given intravenously to try to reveal the Brugada ECG pattern. This test is performed in a hospital setting under doctor supervision.
- Genetic Tests: Blood tests are performed to identify genetic mutations (especially the SCN5A gene) associated with Brugada Syndrome. This test can help in diagnosis, especially for those with a family history of the syndrome.
- Electrophysiological Study (EPStudy): In patients who have experienced serious symptoms such as fainting, electrical pathways inside the heart are examined for risk assessment.
How is Brugada syndrome treated?
There is no permanent cure for Brugada Syndrome, but the most important goal is to prevent dangerous arrhythmias and reduce the risk of sudden death. Treatment is determined according to the patient’s risk level. In high-risk patients, the most effective treatment method is implanting an implantable cardioverter-defibrillator (ICD).
The methods used in Brugada Syndrome treatment are:
- Implantable Cardioverter-Defibrillator (ICD): In patients at high risk of sudden death, ICD is the most reliable treatment method. This small device placed in your chest or under your collarbone continuously monitors your heart’s rhythm. When it detects a dangerous arrhythmia such as VFib, it automatically gives an electrical shock to return heart rhythm to normal and saves lives.
- Drug Therapy: Some anti-arrhythmic drugs (for example, quinidine) can be used alongside ICD in high-risk patients. However, drug therapy alone is not sufficient to reduce sudden death risk.
- Fever Control: Since high fever can trigger dangerous arrhythmias in people with Brugada Syndrome, medications such as paracetamol should be used to reduce fever during febrile illnesses.
- Avoiding Medications: Your doctor will give you a list of medications that can trigger the syndrome. You must definitely avoid these medications.
Nutrition in Brugada syndrome
Nutrition does not directly treat Brugada syndrome; however, protecting your general heart health reduces your arrhythmia risk. Balanced, salt-restricted nutrition emphasizing vegetables and fruits supports heart functions.
Staying away from alcohol, excessive caffeine, energy drinks, and heavy fatty foods can prevent sudden rhythm changes. During febrile illness periods, consuming plenty of fluids and quickly reducing fever is important.
Exercise in Brugada syndrome
Light and moderate-tempo exercises are generally safe, but high-intensity, long-duration competitive sports can trigger arrhythmias.
You must definitely consult with your cardiology specialist before starting an exercise program. Activities such as swimming, walking, yoga both protect your heart health and improve your general condition.
What are the risks of Brugada syndrome?
The most important risk is sudden cardiac arrest. This usually develops as ventricular fibrillation and can be fatal within minutes. Fever, some medications, and electrolyte disorders increase the risk. In undiagnosed patients, these triggers can have serious consequences. Therefore, if you have been diagnosed, you should keep the risky medication list given to you with you.
How can Brugada syndrome be prevented?
What you can do to prevent the risks of Brugada Syndrome:
- If you have been diagnosed with Brugada Syndrome, you should go to regular cardiology examinations.
- When you have a fever, immediately use fever-reducing medications and take care to keep your body temperature at normal levels.
- Get a list of medications that can trigger Brugada Syndrome from your doctor and avoid using these medications.
- If there is a history of Brugada Syndrome or sudden death in your family, ensure that other family members are also checked with genetic screening and ECG.
When should you consult a doctor?
Emergency medical evaluation is required in the following situations:
- If you suddenly faint (syncope) without a history of heart disease
- If abnormal breathing during sleep is noticed
- If there is a history of sudden, unexplained death at a young age in your family
Reference: Brugada Syndrome