A leadless pacemaker is a small cardiac pacing device that is implanted entirely inside the heart, without the need for surgical pockets under the skin or electrical leads running through the veins. It is designed to treat slow heart rhythms (bradycardia) by delivering electrical impulses directly to the heart muscle when the heart’s own rhythm is too slow or unreliable.
Unlike traditional pacemakers, which consist of a generator placed under the skin and one or more wires connected to the heart, a leadless pacemaker is a single, self-contained device placed directly inside the heart using a minimally invasive catheter-based procedure.
- Why Leadless Pacemakers Were Developed
- How a Leadless Pacemaker Works
- Single-Chamber and “Dual-Chamber–Like” Leadless Pacing
- Who Is a Candidate for a Leadless Pacemaker?
- The Leadless Pacemaker Implantation Procedure
- Recovery After Leadless Pacemaker Implantation
- Battery Life and Long-Term Management
- Advantages and Limitations of Leadless Pacemakers
- In Summary
Why Leadless Pacemakers Were Developed
Conventional pacemakers are highly effective, but over time some complications may arise from the device pocket or the pacing leads. These can include infections, lead damage, or problems related to vein access.
Leadless pacemakers were developed to eliminate these components entirely. By removing the need for leads and a surgical pocket, leadless pacing reduces infection risk, avoids vein-related complications, and improves comfort and cosmetic appearance. For many patients, this results in a simpler long-term solution.
How a Leadless Pacemaker Works
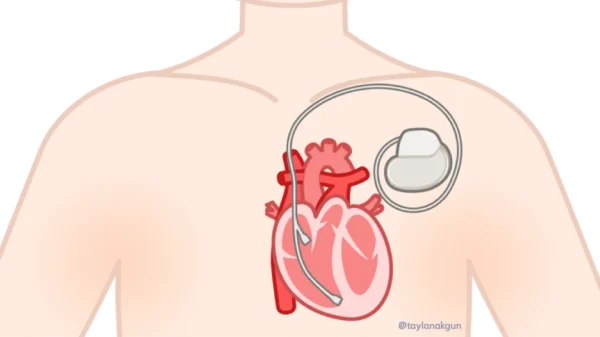
A leadless pacemaker is implanted directly into the right ventricle, the lower pumping chamber of the heart. The device continuously monitors the heart’s electrical activity and delivers pacing impulses only when needed.
All essential components—including the battery, electronics, and pacing electrodes—are contained within a capsule roughly the size of a large vitamin. Once implanted, the device becomes securely attached to the heart muscle and functions automatically in the background.
Single-Chamber and “Dual-Chamber–Like” Leadless Pacing
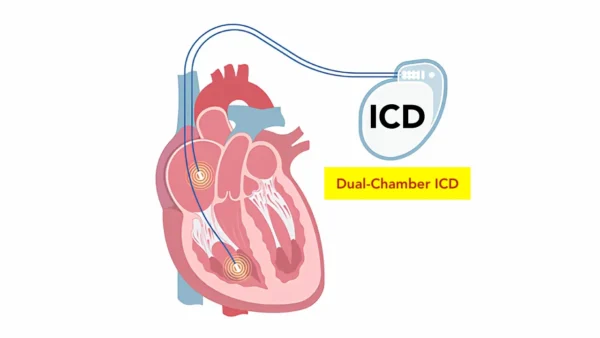
Leadless pacemakers were initially designed for single-chamber ventricular pacing, meaning they stimulate only the lower chamber of the heart. This remains appropriate for many patients, especially those with permanent atrial fibrillation or isolated conduction problems.
More recent leadless systems can also sense atrial activity indirectly by detecting subtle mechanical signals associated with atrial contraction. Although they do not pace the atrium itself, they can time ventricular pacing to follow atrial activity. This allows the device to behave similarly to a dual-chamber pacemaker by preserving coordination between the upper and lower chambers of the heart.
In addition, true dual-chamber leadless pacemaker systems—using two small devices that communicate wirelessly inside the heart—have now become clinically available. These systems allow both atrial and ventricular pacing without traditional leads, further expanding the role of leadless pacing.
Who Is a Candidate for a Leadless Pacemaker?
Leadless pacemakers are suitable for a growing number of patients who need pacing support. They are especially advantageous for individuals with a high risk of infection, limited vein access, prior pacemaker infections, or those receiving long-term dialysis.
Importantly, leadless pacemakers are no longer limited to special or high-risk cases. In many patients with standard single-chamber pacing indications, they may be considered a first-line option, depending on heart rhythm needs and overall clinical evaluation.
The choice between a leadless pacemaker and a traditional system is individualized and based on rhythm type, pacing requirements, anatomy, and long-term considerations.
The Leadless Pacemaker Implantation Procedure
Leadless pacemaker implantation is performed in a cardiac catheterization or electrophysiology laboratory, usually under local anesthesia with light sedation.
The device is delivered through a catheter inserted into a vein in the groin and guided into the heart under imaging. Once the pacemaker is positioned correctly, its electrical performance is tested, and it is securely attached to the heart wall.
There is no chest incision, and the procedure typically takes less than one hour.
Recovery After Leadless Pacemaker Implantation
Recovery is generally quick and uncomplicated. Most patients remain under observation overnight and return home the next day.
Because there is no surgical pocket or chest incision, discomfort is minimal, and restrictions on arm movement are not required. Patients are usually advised to avoid heavy physical activity for a short period while the groin access site heals.
Battery Life and Long-Term Management
The battery life of a leadless pacemaker depends on how often pacing is needed and how the device is programmed. In clinical studies, projected battery longevity is commonly around 8 to 10 years, though this may vary from patient to patient.
When the battery is nearing depletion, the most common approach is to deactivate the existing device and implant a new leadless pacemaker at a different location within the heart. In most cases, the original device is safely left in place.
In selected situations—such as infection or other complications—the older device may need to be removed. This decision is made on an individual basis.
Advantages and Limitations of Leadless Pacemakers
Leadless pacemakers offer clear benefits, including lower infection risk, avoidance of lead-related problems, and improved comfort. However, they are not suitable for every patient.
They are currently not used for therapies that require pacing of both ventricles, such as cardiac resynchronization therapy, and some patients still benefit more from conventional pacemaker systems. Careful evaluation ensures the most appropriate device choice.
In Summary
A leadless pacemaker is a modern pacing device implanted entirely inside the heart, offering an effective and less invasive alternative to traditional pacemakers. While initially limited to single-chamber pacing, newer technologies now allow preservation of atrioventricular coordination and even true dual-chamber leadless pacing in selected patients. When chosen appropriately, leadless pacemakers provide reliable rhythm support with fewer long-term device-related complications and excellent patient comfort.
Reference: Leadless Pacemakers