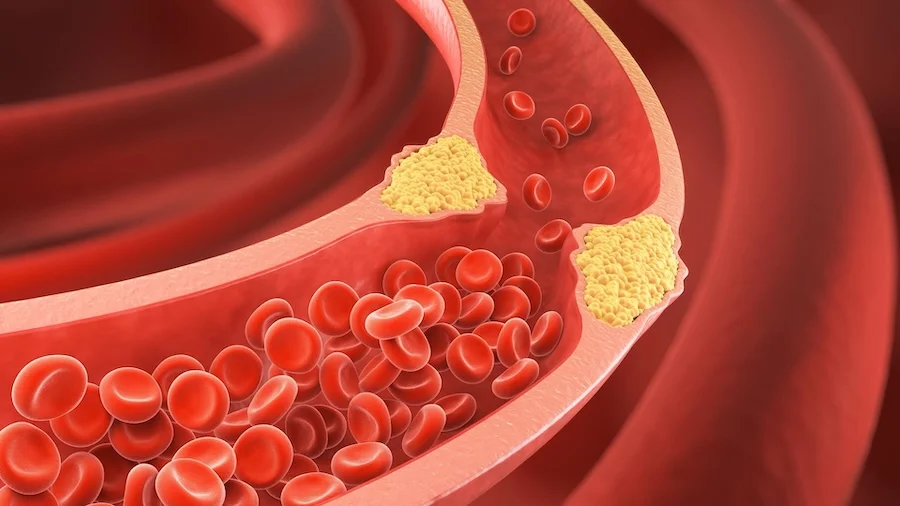
Atherosclerosis is a condition in which fatty deposits, cholesterol, and inflammatory material build up inside the walls of arteries, forming plaques that narrow and stiffen the vessels. Over time, this process restricts blood flow and reduces oxygen delivery to vital organs such as the heart, brain, and limbs.
Atherosclerosis develops gradually over many years and often causes no symptoms until it becomes advanced. It is the underlying cause of many serious cardiovascular diseases, including heart attacks, strokes, and peripheral artery disease.
How Atherosclerosis Develops
Healthy arteries are flexible and allow blood to flow freely. Atherosclerosis begins when the inner lining of the artery is damaged. This damage allows cholesterol—particularly low-density lipoprotein (LDL)—to penetrate the vessel wall.
The body responds with inflammation. Immune cells enter the artery wall, ingest cholesterol, and form fatty streaks. Over time, these areas grow into plaques composed of fat, inflammatory cells, calcium, and fibrous tissue. As plaques enlarge, arteries become narrower and less elastic.
Some plaques remain stable, while others become fragile and prone to rupture. Plaque rupture can trigger sudden clot formation, leading to abrupt blockage of blood flow.
Why Atherosclerosis Is Dangerous
Atherosclerosis can limit blood flow gradually or cause sudden, complete blockage when a plaque ruptures and a clot forms. The consequences depend on which artery is affected.
Reduced blood flow to the heart can cause chest pain or heart attack. Blockage in brain arteries can result in stroke. Narrowing of leg arteries may lead to pain with walking and poor wound healing.
Because atherosclerosis often progresses silently, serious complications may be the first sign of disease.
Common Risk Factors for Atherosclerosis
Atherosclerosis develops due to a combination of genetic, metabolic, and lifestyle factors.
Major risk factors include high cholesterol levels, high blood pressure, smoking, diabetes, obesity, physical inactivity, and advancing age. A family history of early cardiovascular disease also increases risk.
The presence of multiple risk factors accelerates plaque formation and progression.
Symptoms of Atherosclerosis
Symptoms depend on the location and severity of arterial narrowing.
Many people have no symptoms for years. When symptoms occur, they are usually related to reduced blood flow, such as chest pain with exertion, shortness of breath, leg pain while walking, dizziness, or sudden neurological symptoms.
Symptom onset often indicates advanced disease.
How Atherosclerosis Is Diagnosed
Diagnosis is based on risk assessment, clinical evaluation, and imaging.
Blood tests assess cholesterol and metabolic risk factors. Imaging studies such as ultrasound, CT scans, or angiography may be used to visualize plaque buildup and assess blood flow.
In many cases, atherosclerosis is identified indirectly after a cardiovascular event rather than through routine screening.
Treatment Options for Atherosclerosis
Treatment focuses on slowing disease progression, stabilizing plaques, and reducing the risk of cardiovascular events.
Lifestyle Modification
Lifestyle changes are the foundation of atherosclerosis management. Heart-healthy nutrition, regular physical activity, smoking cessation, weight management, and stress reduction significantly reduce cardiovascular risk.
These measures improve cholesterol levels, blood pressure, and overall vascular health.
Medical Therapy
Medications play a key role in controlling risk factors. Drugs used to lower cholesterol, control blood pressure, manage diabetes, and reduce clot formation help stabilize plaques and prevent complications.
Medical therapy is usually long-term and often lifelong.
Interventional and Surgical Treatments
When atherosclerosis leads to significant narrowing or blockage of arteries and causes symptoms or threatens organ function, interventional or surgical treatment may be required to restore blood flow.
The choice of procedure depends on the location of the diseased artery, the extent of plaque buildup, symptom severity, and the patient’s overall health.
Percutaneous Coronary Intervention (Angioplasty and Stenting)
Percutaneous coronary intervention (PCI) is a minimally invasive, catheter-based procedure commonly used to treat narrowed or blocked coronary arteries.
During angioplasty, a small balloon is inflated inside the narrowed artery to compress the plaque and widen the vessel. In most cases, a stent (a small metal mesh tube) is then placed to keep the artery open and improve long-term blood flow.
This approach is widely used in patients with coronary artery disease, especially those with chest pain or heart attack related to atherosclerosis.
Peripheral Artery Interventions
For atherosclerosis affecting arteries outside the heart—such as the legs—similar catheter-based techniques may be used.
These procedures include balloon angioplasty, stent placement, or specialized devices designed to remove or modify plaque. They aim to relieve symptoms such as leg pain with walking and improve circulation.
Carotid Artery Revascularization
When atherosclerosis affects the carotid arteries supplying the brain, treatment may be needed to reduce stroke risk.
Options include carotid endarterectomy, a surgical procedure that removes plaque directly from the artery, or carotid artery stenting, a less invasive catheter-based approach used in selected patients.
Coronary Artery Bypass Surgery
Coronary artery bypass grafting (CABG) is a surgical procedure used in patients with extensive or complex coronary artery disease.
In this operation, blood vessels from other parts of the body are used to create new pathways that bypass severely narrowed or blocked coronary arteries, restoring blood flow to the heart muscle.
CABG is often recommended for patients with multivessel disease, left main coronary artery disease, or when catheter-based treatments are not suitable.
Choosing the Appropriate Approach
No single treatment is right for every patient. Decisions are based on anatomy, disease severity, symptom burden, procedural risk, and long-term benefit.
Interventional and surgical treatments are typically combined with ongoing medical therapy and lifestyle modification, as procedures treat existing blockages but do not cure atherosclerosis itself.
Preventing Progression of Atherosclerosis
Atherosclerosis is largely preventable and manageable with early intervention. Controlling risk factors before symptoms develop significantly reduces the likelihood of heart attack or stroke.
Even after diagnosis, aggressive risk factor management can halt progression and improve outcomes.
In Summary
Atherosclerosis is a chronic inflammatory disease characterized by plaque buildup within arterial walls. It develops silently over time and underlies many serious cardiovascular conditions. By addressing risk factors through lifestyle changes, medications, and—when necessary—procedures, the progression of atherosclerosis can be slowed and its complications largely prevented.
Reference: Atherosclerosis