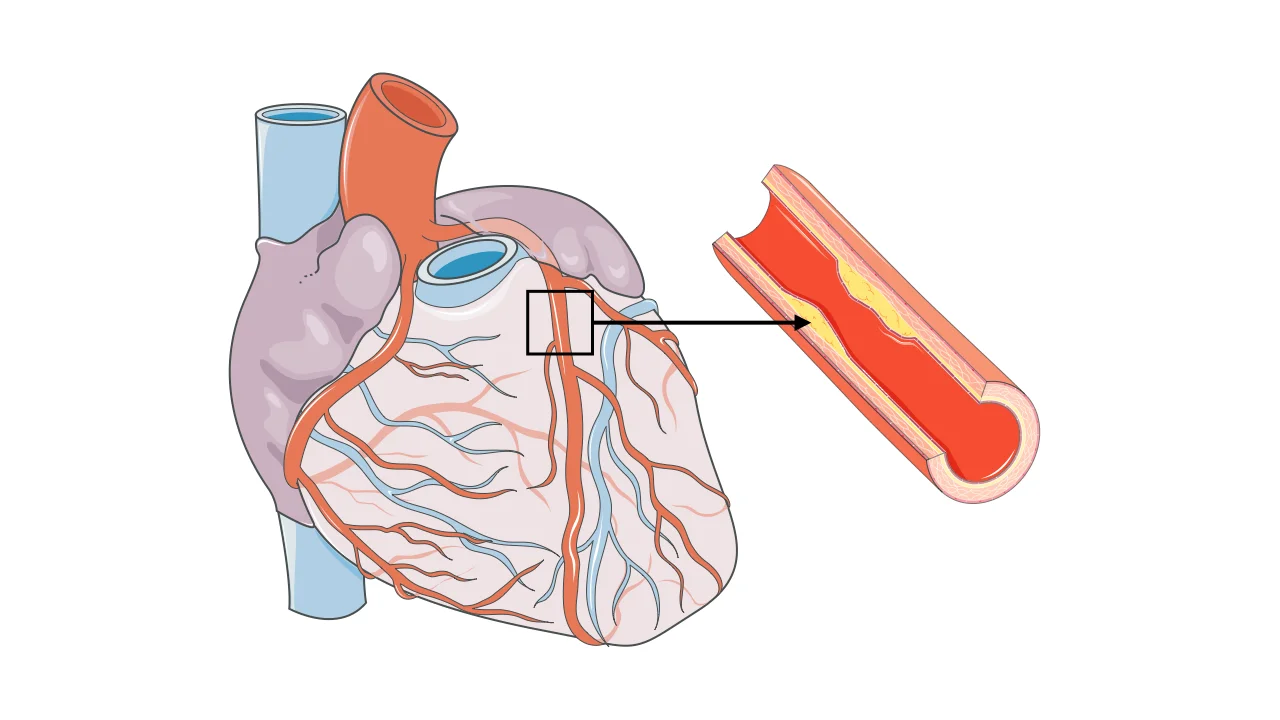
Coronary artery disease (CAD) is a condition in which the blood vessels that supply the heart muscle become narrowed or blocked by fatty deposits called plaques. These arteries, known as the coronary arteries, are responsible for delivering oxygen-rich blood to the heart. When blood flow is reduced, the heart muscle may not receive enough oxygen, particularly during physical or emotional stress.
CAD is the most common form of heart disease worldwide and a leading cause of heart attacks and heart failure. Understanding how it develops—and how it affects the heart—is essential for prevention, early diagnosis, and effective treatment.
How Coronary Artery Disease Develops
Coronary artery disease develops gradually through a process called atherosclerosis. This process begins when the inner lining of a coronary artery becomes damaged, often due to risk factors such as high cholesterol, smoking, high blood pressure, or diabetes.
Over time, cholesterol, inflammatory cells, and fibrous tissue accumulate within the artery wall, forming atherosclerotic plaques. As these plaques grow, they narrow the artery and restrict blood flow to the heart muscle. When oxygen demand increases—such as during physical activity or emotional stress—the reduced blood flow may cause symptoms.
In some cases, a plaque can rupture suddenly. This triggers the formation of a blood clot that may completely block the artery, leading to a heart attack. This sudden event explains why coronary artery disease can remain silent for years and then present abruptly.
Symptoms of Coronary Artery Disease
Symptoms of coronary artery disease vary widely. Some people have no symptoms for years, while others experience clear warning signs.
The most common symptom is chest discomfort, often described as pressure, tightness, or heaviness. This discomfort may spread to the arms, neck, jaw, back, or upper abdomen. Symptoms often occur with exertion or stress and improve with rest.
Other symptoms may include:
- Shortness of breath
- Fatigue with activity
- Nausea or sweating
- Dizziness
In some individuals—especially people with diabetes—symptoms may be mild or atypical.
Why Coronary Artery Disease Is Dangerous
Reduced blood flow to the heart muscle can weaken its function over time, contributing to Heart Failure. More urgently, sudden blockage of a coronary artery can cause a heart attack, permanently damaging heart muscle.
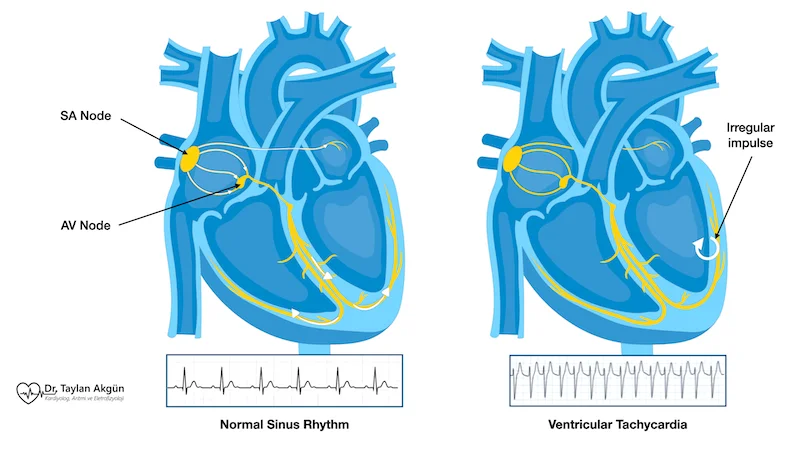
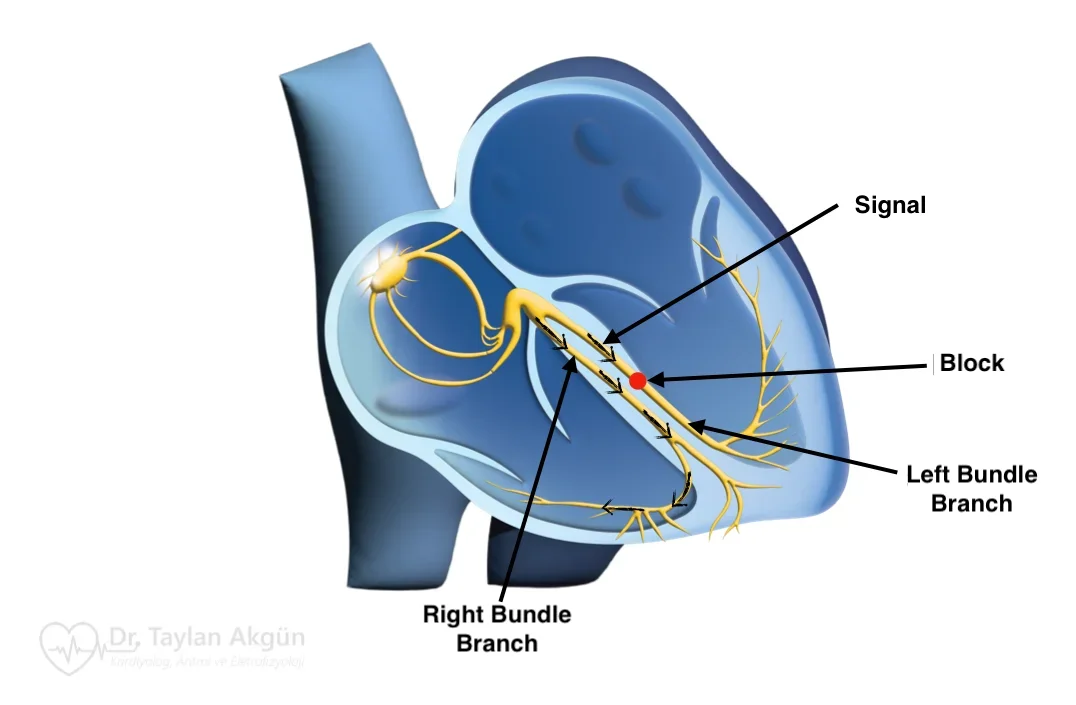
CAD is also closely linked to dangerous heart rhythm disturbances. Scar tissue formed after a heart attack increases the risk of ventricular arrhythmias and Sudden Cardiac Arrest.
Risk Factors for Coronary Artery Disease
CAD is influenced by both lifestyle and genetic factors.
Common risk factors include high blood pressure, high cholesterol, diabetes, smoking, obesity, physical inactivity, and chronic stress. Age and family history also play important roles.
The good news is that many risk factors are modifiable. Addressing them can slow disease progression and significantly reduce the risk of complications.
How Coronary Artery Disease Is Diagnosed
Diagnosis begins with a detailed clinical assessment and evaluation of symptoms and risk factors. Noninvasive tests may be used to assess blood flow to the heart during rest and stress.
Imaging studies help identify narrowed or blocked arteries and assess heart muscle function. In some cases, coronary angiography is performed to directly visualize the coronary arteries and determine the severity and location of blockages.
The goal of diagnostic testing is to confirm CAD, assess risk, and guide treatment decisions.
Treatment Options for Coronary Artery Disease
Treatment of coronary artery disease focuses on three main goals:
improving blood flow to the heart, relieving symptoms, and preventing heart attacks and long-term complications. Most patients require a combination of lifestyle changes, medications, and—in selected cases—procedural treatment.
Lifestyle and Risk Factor Management
Lifestyle modification is the foundation of CAD treatment and remains essential even when medications or procedures are used.
Stopping smoking is one of the most powerful interventions, as smoking directly accelerates atherosclerosis and increases clot formation. A heart-healthy diet helps lower cholesterol levels and reduce plaque progression. Regular physical activity improves cardiovascular fitness, insulin sensitivity, and blood pressure control.
Weight management and stress reduction also play important roles. These measures do not simply improve symptoms; they slow disease progression and reduce the risk of future cardiac events.
Medication Therapy
Medications are central to the long-term management of coronary artery disease and are prescribed to address different aspects of the disease process.
Some medications lower cholesterol levels and stabilize atherosclerotic plaques, reducing the risk of plaque rupture. Others control blood pressure and decrease the heart’s workload, allowing the heart muscle to function more efficiently. Antiplatelet medications reduce the risk of blood clot formation within narrowed arteries.
Together, these therapies significantly reduce the risk of heart attack, stroke, and death, even in patients who do not have prominent symptoms.
Procedures to Restore Blood Flow
In some patients, lifestyle changes and medications are not sufficient to control symptoms or reduce risk. In these situations, procedures aimed at restoring blood flow to the heart muscle may be recommended.
One common approach is coronary angioplasty, also known as percutaneous coronary intervention (PCI). During this minimally invasive procedure, a thin catheter is advanced through a blood vessel—usually from the wrist or groin—to the narrowed coronary artery. A small balloon is then inflated to open the blockage and improve blood flow.
In most cases, a stent is placed at the treated site. A stent is a small metal mesh tube that remains inside the artery to keep it open and reduce the risk of re-narrowing. Modern stents are often coated with medication to further lower the chance of future blockage.
In patients with more extensive or complex coronary artery disease—such as multiple severe blockages or involvement of critical artery segments—coronary artery bypass surgery may be recommended. This surgical approach creates new pathways for blood to flow around blocked arteries.
These procedures can significantly relieve symptoms and improve quality of life. In selected high-risk patients, they may also improve survival. However, it is important to understand that procedures treat existing blockages but do not cure the underlying atherosclerosis. Long-term medical therapy and lifestyle modification remain essential after any intervention.
Choosing the Right Treatment Strategy
The choice of treatment depends on several factors, including symptom severity, the extent and location of coronary artery disease, heart function, and overall health.
Some patients do very well with lifestyle changes and medications alone. Others benefit from a combination of medical and procedural therapy. Treatment decisions are individualized and often involve shared decision-making between the patient and the care team.
Living With Coronary Artery Disease
A diagnosis of coronary artery disease does not mean life must slow down. With appropriate treatment and lifestyle changes, many people live active and fulfilling lives.
Regular follow-up, adherence to treatment, and attention to symptoms are essential. Early recognition of changes can prevent serious complications.
In Summary
Coronary artery disease is caused by narrowing or blockage of the arteries that supply the heart muscle. It develops gradually but can lead to heart attack, heart failure, and serious rhythm disturbances. Early diagnosis, aggressive risk factor management, and individualized treatment are key to living well with CAD.
Reference: Coronary artery disease