Arrhythmias are conditions in which the heart beats too fast, too slow, or in an irregular pattern. While the word “arrhythmia” may sound alarming, not all rhythm disturbances are dangerous. Some are harmless and temporary, while others require careful evaluation and treatment.
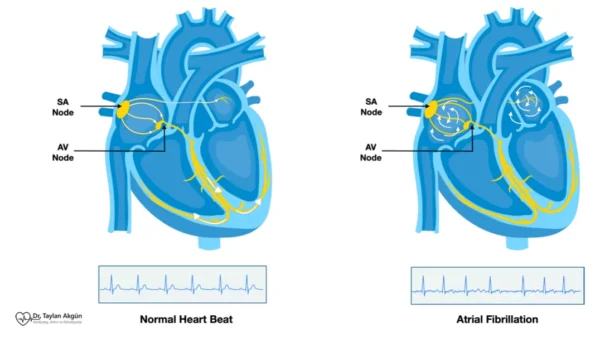
The heart is more than a muscle—it is also an electrical organ. Arrhythmias occur when the electrical signals that coordinate each heartbeat are disrupted. Understanding this electrical aspect is essential to understanding why arrhythmias happen, how they feel, and how they are treated.
How the Heart’s Rhythm Is Normally Controlled
Each heartbeat is triggered by a carefully timed electrical signal that starts in the heart’s natural pacemaker. This signal travels through a defined pathway, allowing the heart chambers to contract in a precise sequence. This coordination ensures that blood flows efficiently to the lungs and the rest of the body.
When this electrical system functions properly, the heartbeat is steady and responsive, speeding up during activity and slowing down at rest. Arrhythmias arise when signals follow the wrong path, occur too frequently, too slowly, or become disorganized.
What an Arrhythmia Feels Like
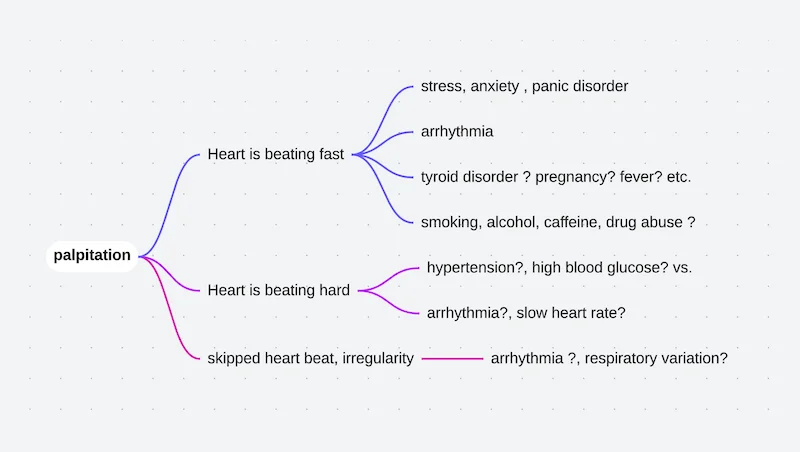
The experience of an arrhythmia varies widely. Some people feel every abnormal beat, while others may be unaware that anything is wrong. Symptoms can come and go or persist over time.
Before listing common symptoms, it is important to note that symptom severity does not always reflect risk. Mild sensations can sometimes accompany serious rhythms, while dramatic palpitations may be caused by benign conditions.
Common symptoms include:
- Palpitations or awareness of the heartbeat
- A racing, fluttering, or irregular sensation in the chest
- Shortness of breath
- Fatigue or reduced exercise tolerance
- Dizziness or lightheadedness
- Chest discomfort
In some cases, arrhythmias can cause fainting or near-fainting, particularly when blood flow to the brain is temporarily reduced.
Why Arrhythmias Occur
Arrhythmias can develop for many reasons. Some originate from changes within the heart itself, while others are triggered by conditions affecting the entire body.
Heart-related causes include structural heart disease, scarring from previous heart attacks, valve disorders, and age-related changes in the heart’s electrical system. Non-cardiac factors such as thyroid disorders, electrolyte imbalances, infections, dehydration, anemia, and certain medications can also provoke rhythm disturbances.
Lifestyle factors—including stress, poor sleep, caffeine, alcohol, and stimulant use—may trigger or worsen arrhythmias in susceptible individuals.
Major Types of Arrhythmias
Arrhythmias are broadly categorized based on where in the heart they originate and how they affect the heart rate.
Some arrhythmias cause the heart to beat too fast. These are known as tachyarrhythmias and include conditions such as Supraventricular Tachycardia, Atrial Fibrillation, and Ventricular Tachycardia. Their seriousness varies greatly depending on their origin and mechanism.
Other arrhythmias slow the heart rate. These are called bradyarrhythmias and often result from problems in the heart’s conduction system, such as Heart Block. Mild forms may be harmless, while advanced forms may require pacing therapy.
Some rhythm disturbances are irregular but not necessarily fast or slow. These include premature beats, which are common and often benign, though they can feel unsettling.
How Arrhythmias Are Diagnosed
Diagnosing an arrhythmia requires documenting the heart’s electrical activity. An electrocardiogram is the primary tool, but because arrhythmias may be intermittent, longer-term monitoring is often necessary.
Additional tests may be used to evaluate heart structure, blood flow, and potential triggers. The goal is not only to identify the rhythm itself, but also to understand why it is occurring and whether it poses a risk.
When Arrhythmias Are Concerning
Many arrhythmias are harmless and require little more than reassurance. Concern increases when an arrhythmia causes significant symptoms, occurs frequently, lasts for prolonged periods, or is associated with underlying heart disease.
Certain arrhythmias increase the risk of stroke, heart failure, or sudden cardiac events. Identifying these higher-risk rhythms is a key part of evaluation and guides treatment decisions.
Treatment Principles for Arrhythmias
Treatment of arrhythmias is always individualized because not all rhythm disturbances behave the same way or carry the same risk. In some people, reassurance and follow-up are all that is needed. In others, treatment is aimed at relieving symptoms, preventing complications, or protecting the heart from dangerous rhythm disturbances.
The choice of treatment depends on several factors, including the type of arrhythmia, how often it occurs, whether it causes symptoms, and whether there is underlying heart disease.
Medications
Medications are often the first step in managing arrhythmias. Some drugs are used to slow the heart rate when it beats too fast, helping the heart fill and pump more efficiently. Others are designed to stabilize the heart’s electrical activity and reduce the likelihood of abnormal rhythms occurring.
In certain arrhythmias, especially those that increase the risk of stroke, medications may also be prescribed to reduce blood clot formation. These treatments do not correct the rhythm itself but play a critical role in preventing serious complications.
The goal of medication therapy is symptom control and risk reduction, not necessarily eliminating every abnormal heartbeat.
Cardioversion
In some arrhythmias, particularly those that persist and do not stop on their own, restoring a normal rhythm may be recommended. Cardioversion is a controlled medical procedure that resets the heart’s rhythm either with medication or a brief, carefully delivered electrical impulse.
The procedure is performed under short-acting anesthesia, so the patient does not feel pain. Cardioversion does not cure the underlying cause of the arrhythmia, but it can restore a normal rhythm and improve symptoms, often allowing other treatments to work more effectively afterward.
Catheter Ablation
For certain arrhythmias, the problem lies in a specific abnormal electrical pathway or trigger within the heart. Catheter ablation is a procedure designed to locate and eliminate this source.
During ablation, thin catheters are guided through blood vessels to the heart. Using detailed electrical mapping, the abnormal area is identified and treated with controlled energy to prevent it from generating or conducting faulty signals. Once successfully treated, the arrhythmia may not return.
Ablation is considered a definitive treatment for many rhythm disorders and can significantly reduce or eliminate the need for long-term medication.
Implantable Devices
Some arrhythmias cause the heart to beat too slowly or interrupt electrical conduction between heart chambers. In these cases, the heart may not maintain a reliable rhythm on its own.
A Pacemaker is a small implanted device that provides consistent electrical signals to keep the heart beating at an appropriate rate. It does not cure the underlying electrical disease but ensures that the heart rhythm remains safe and stable.
In patients at risk of dangerous fast rhythms originating from the ventricles, a different device called an Implantable Cardioverter-Defibrillator may be recommended. This device continuously monitors the heart rhythm and can deliver life-saving therapy if a serious arrhythmia occurs.
Lifestyle Modifications and Risk Reduction
Medical treatments are only one part of arrhythmia management. Daily habits and underlying health factors play a powerful role in how often arrhythmias occur, how severe they feel, and how well treatments work.
Maintaining a healthy body weight reduces strain on the heart and lowers the likelihood of rhythm disturbances. Regular, moderate physical activity helps stabilize heart rate and improves overall cardiovascular health, while extreme or unaccustomed exertion should be approached cautiously in people with known arrhythmias.
Limiting stimulants such as caffeine and avoiding excessive alcohol intake can significantly reduce palpitations in many individuals. Adequate sleep and stress management are equally important, as poor sleep quality and chronic stress can trigger or worsen abnormal rhythms.
Treating contributing conditions—such as high blood pressure, diabetes, thyroid disorders, and sleep apnea—is essential. These conditions do not simply coexist with arrhythmias; they often drive their development and progression. Addressing them improves rhythm control and reduces long-term complications.
Lifestyle changes do not replace medical therapy when it is needed, but they enhance its effectiveness and, in some cases, reduce the need for more aggressive treatments.
Stroke Prevention Strategies
Some arrhythmias, especially those involving disorganized atrial activity, increase the risk of stroke. In addition to medications, certain patients may benefit from procedures designed to reduce this risk when long-term blood-thinning therapy is not suitable.
These approaches focus on preventing clot formation in areas of the heart where blood can pool during abnormal rhythms. While they do not treat the arrhythmia itself, they address one of its most serious consequences.
Living With an Arrhythmia
Being told you have an arrhythmia can be unsettling. Education plays a critical role in reducing fear and uncertainty. Understanding what type of arrhythmia is present, what triggers it, and how it is managed empowers patients to participate actively in their care.
With proper evaluation, follow-up, and individualized treatment, most people with arrhythmias can live full and active lives.
In Summary
Arrhythmias are disorders of the heart’s electrical system that can cause the heart to beat too fast, too slow, or irregularly. While many arrhythmias are benign, others require careful attention. Accurate diagnosis, understanding the underlying cause, and tailoring treatment to the individual allow most patients to manage arrhythmias safely and confidently.
You may also like to read these:
Premature Beats (PACs and PVCs)
Supraventricular Tachycardia (SVT)
AV Nodal Reentrant Tachycardia (AVNRT)
WPW Syndrome (Wolff-Parkinson-White)
Reference: Arrhythmias