Most of the time, you’re completely unaware of your heartbeat. But sometimes you suddenly feel your heart pounding, racing, fluttering, or skipping beats in your chest. These sensations, called palpitations, can be alarming—especially the first time you experience them. The good news is that palpitations are extremely common and usually harmless, even though they feel concerning. Nearly everyone experiences them at some point, and they rarely indicate serious heart problems.
Overview
Heart palpitations are the awareness of your own heartbeat. You notice sensations you normally don’t feel—your heart beating, pounding, racing, fluttering, skipping, or thumping in your chest, throat, or neck. These sensations can last seconds, minutes, or occasionally longer.
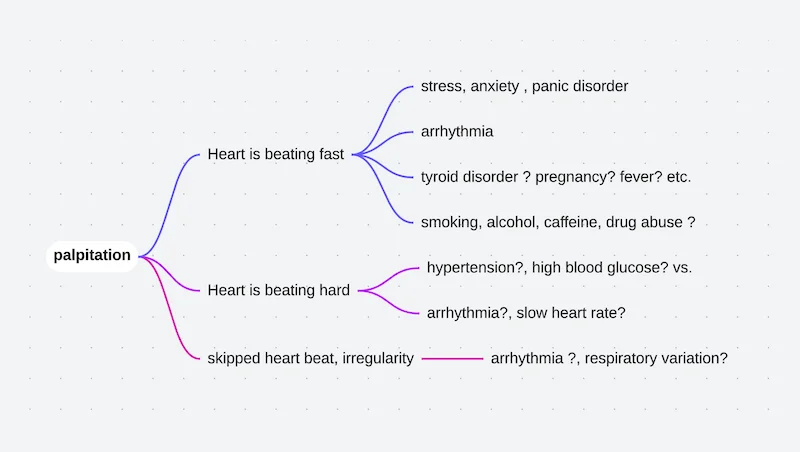
The key point is that palpitations are a symptom, not a diagnosis. They describe what you’re feeling, not what’s actually happening with your heart rhythm. Sometimes palpitations occur with completely normal heart rhythm—you’re simply more aware of normal beats. Other times they indicate actual rhythm abnormalities ranging from harmless extra beats to more significant arrhythmias.
Common descriptions of palpitations vary between individuals. Some feel their heart “racing” or beating very fast. Others notice a “fluttering” or “flip-flopping” sensation, like a fish or butterfly in their chest. Many describe “skipped beats” or pauses, though the heart rarely actually skips—instead, an early beat is followed by a pause, creating the sensation of skipping. Some notice strong, forceful beats or pounding, particularly in their neck or throat. A few feel vibrating or quivering sensations.
Palpitations occur in various patterns. Occasional isolated palpitations lasting seconds are most common. Some people experience brief episodes lasting minutes. Others have persistent awareness of their heartbeat for hours or days. The pattern helps identify the cause.
Most palpitations are benign, meaning they pose no health risk. Premature beats, where the heart contracts slightly early, account for many palpitations and are completely harmless in people with normal hearts. Sinus tachycardia, where your heart appropriately speeds up in response to triggers, causes palpitations but isn’t dangerous. Even some abnormal rhythms causing palpitations aren’t life-threatening, though they may need treatment for symptom relief.
The challenge is that palpitations feel the same whether they’re from harmless extra beats or more serious rhythm problems. Your sensation alone can’t distinguish benign from concerning causes. This is why evaluation is often recommended, particularly for new or concerning palpitations.
Causes
Palpitations result from numerous causes, most of which are harmless.
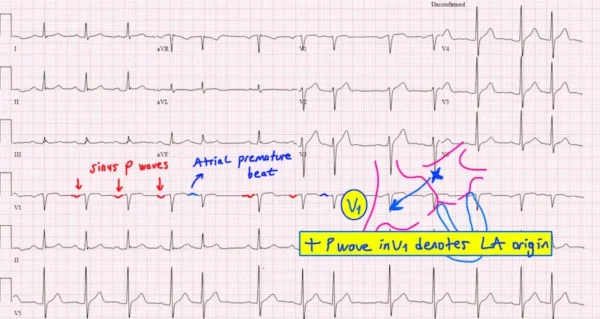
- Premature beats are the most common cause. These extra heartbeats occur slightly earlier than expected, briefly interrupting normal rhythm. Premature atrial contractions originate in the upper chambers, while premature ventricular contractions come from the lower chambers. Both create similar sensations—a flutter, thump, or skipped beat feeling. Nearly everyone has thousands of these daily without noticing most of them.
- Stress and anxiety are major triggers. When you’re anxious or stressed, your body releases adrenaline, which makes you more aware of your heartbeat and can trigger extra beats. The sensation of palpitations then increases anxiety, releasing more adrenaline in a difficult cycle. Panic attacks often cause intense palpitations along with other symptoms.
- Caffeine stimulates your nervous system and can trigger palpitations. Coffee, tea, energy drinks, sodas, chocolate, and some medications contain caffeine. Sensitivity varies enormously—some people tolerate large amounts without problems, while others develop palpitations from minimal caffeine.
- Nicotine from smoking or vaping increases heart rate and can trigger palpitations and extra beats.
- Alcohol, particularly in excess, commonly causes palpitations during consumption and during withdrawal. Even moderate drinking triggers palpitations in sensitive individuals.
- Dehydration and electrolyte imbalances affect heart rhythm. Low potassium or magnesium levels particularly trigger extra beats. This is why palpitations sometimes occur after intense exercise with heavy sweating.
- Medications commonly cause palpitations. Decongestants containing pseudoephedrine, asthma inhalers, thyroid medications, some blood pressure drugs, and certain antidepressants all can trigger palpitations. Even some herbal supplements act as stimulants.
- Hormonal changes influence palpitations. Many women notice more palpitations during menstrual periods, pregnancy, or menopause. Thyroid problems, particularly hyperthyroidism, cause persistent palpitations.
- Fever and illness increase metabolic demands and heart rate, often making you more aware of your heartbeat.
- Low blood sugar from diabetes medications, skipping meals, or excessive insulin can trigger palpitations as your body releases stress hormones.
- Vigorous exercise increases heart rate dramatically, and you become very aware of your pounding heartbeat. This is normal, though palpitations persisting long after exercise ends warrant evaluation.
- Digestive issues occasionally trigger palpitations. Large meals, gas, bloating, or acid reflux might stimulate the vagus nerve, which affects both digestion and heart rate.
- Sleep deprivation and fatigue make palpitations more likely and noticeable.
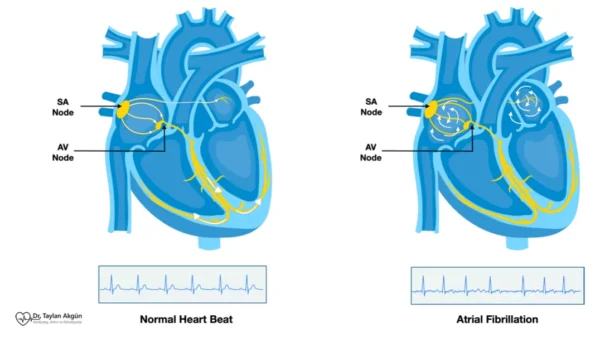
- Heart rhythm abnormalities cause some palpitations. Atrial fibrillation creates irregular, often rapid rhythm. Supraventricular tachycardia causes sudden episodes of very rapid heartbeat. These conditions need medical evaluation.
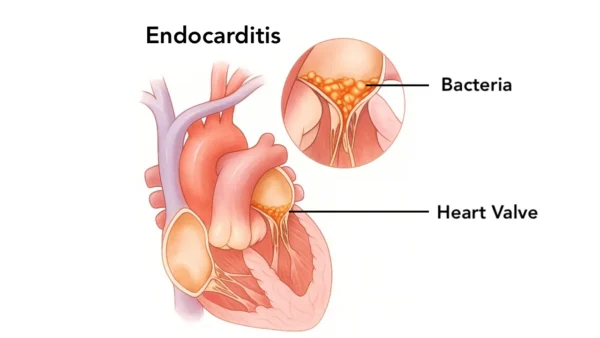
- Rarely, serious heart conditions including valve disease, cardiomyopathy, or coronary artery disease cause palpitations, usually accompanied by other symptoms.
Symptoms
The sensation of palpitations varies widely between individuals and even between episodes in the same person.
- Awareness of heartbeat is the defining feature. You suddenly notice your heart beating when you normally wouldn’t. This awareness alone can be disconcerting.
- Racing or rapid heartbeat feels like your heart is beating very fast. Your heart rate might actually be elevated, or you might simply be more aware of a normal rate.
- Fluttering sensations feel like rapid, light beating, quivering, or trembling in your chest. Many describe this as butterflies or a bird flapping in the chest.
- Pounding or thumping means you feel strong, forceful heartbeats. Each beat feels harder or more noticeable than usual. You might feel this in your chest, throat, neck, or even your ears.
- Skipped beats or pauses create the sensation that your heart stopped briefly or missed a beat. Usually, an extra early beat is followed by a compensatory pause, creating this feeling.
- Irregular rhythm means you notice that beats aren’t coming at regular intervals—some seem closer together, others farther apart.
- Location of sensation varies. Most people feel palpitations in their chest, but many notice them in their throat or neck. Some feel palpitations in their upper abdomen.
- Associated symptoms sometimes accompany palpitations. Lightheadedness or dizziness can occur, particularly with very rapid rates. Shortness of breath might develop, especially if palpitations are sustained. Chest discomfort or pressure occasionally accompanies palpitations. Anxiety is common, both as a cause and effect of palpitations.
- Duration varies dramatically. Some palpitations last only seconds—you notice a few irregular beats, then normal rhythm resumes. Others persist for minutes to hours. Very brief episodes are usually less concerning than sustained palpitations.
- The pattern of onset and offset provides clues. Sudden onset and termination suggest certain rhythm problems like supraventricular tachycardia. Gradual onset and offset are more typical of sinus tachycardia or anxiety.
- Many people feel perfectly fine between episodes, even if palpitations are frequent.
Diagnosis
Diagnosing the cause of palpitations involves determining what’s actually happening with your heart rhythm when you feel symptoms.
- Your description is invaluable. Your doctor asks when palpitations occur, how long they last, what they feel like, whether onset is sudden or gradual, what triggers them, what makes them stop, and whether you have other symptoms. This information often points toward likely causes.
- Physical examination includes checking your heart rate and rhythm, listening to your heart for murmurs or irregular beats, checking blood pressure, and looking for signs of thyroid disease or other conditions.
- An electrocardiogram captures your heart’s electrical activity but only for about 10 seconds. If you’re having palpitations during this brief recording, it shows exactly what rhythm is present. However, most palpitations are intermittent, so a standard electrocardiogram often appears completely normal despite frequent symptoms.
- Extended monitoring helps capture intermittent palpitations. Holter monitors worn for 24-48 hours record your heart continuously. You keep a diary noting when you feel palpitations, allowing correlation between symptoms and actual rhythm. Event monitors worn for weeks or months record when you press a button during symptoms or automatically when detecting abnormal rhythms. Smartphone apps that record electrocardiograms during episodes are increasingly useful.
- The goal of monitoring is capturing your rhythm during symptoms. Feeling palpitations while the monitor records shows exactly what’s happening—whether it’s normal rhythm, extra beats, or abnormal rhythms.
- Blood tests identify underlying causes. Thyroid function tests check for hyperthyroidism. Electrolyte panels measure potassium and magnesium. Blood counts detect anemia. Blood sugar levels identify hypoglycemia.
- Echocardiography visualizes your heart’s structure and function using ultrasound. This test identifies structural problems like valve disease or weakened heart muscle that might cause palpitations. In most people with palpitations, the echocardiogram is completely normal, which is reassuring.
- Exercise stress testing evaluates whether physical activity triggers palpitations or reveals underlying heart disease. This is particularly important if palpitations occur during or after exercise.
- If initial testing doesn’t capture the cause and palpitations are frequent or concerning, longer-term monitoring with implantable loop recorders might be recommended. These small devices placed under chest skin monitor rhythm for up to three years.
Treatment
Treatment depends entirely on what’s causing your palpitations.
- For benign causes like occasional premature beats or sinus tachycardia from anxiety, reassurance is often the only treatment needed. Understanding that palpitations are harmless frequently reduces their frequency because anxiety about them decreases.
- Lifestyle modifications help many people. Reducing or eliminating caffeine significantly reduces palpitations in sensitive individuals. Limiting alcohol, particularly if it triggers your symptoms, helps. Staying well-hydrated maintains electrolyte balance. Getting adequate sleep reduces palpitations related to fatigue. Managing stress through relaxation techniques, exercise, meditation, or counseling addresses anxiety-triggered palpitations.
- Treating underlying causes resolves related palpitations. Correcting thyroid problems with medication normalizes heart rhythm. Treating anemia eliminates compensatory increases in heart rate. Managing anxiety with therapy or medication reduces anxiety-related palpitations. Adjusting medications causing palpitations as side effects might eliminate symptoms.
- For people with frequent premature beats causing significant symptoms despite normal heart structure, medications might help. Beta-blockers reduce extra beats and make remaining ones less noticeable by blocking adrenaline effects. However, most doctors avoid medicating benign premature beats unless they’re extremely frequent or highly symptomatic.
- Specific arrhythmias require targeted treatment. Atrial fibrillation needs rate control medications, possibly blood thinners, and consideration of rhythm control strategies. Supraventricular tachycardia might be managed with vagal maneuvers, medications, or catheter ablation. Ventricular tachycardia requires careful evaluation and often aggressive treatment.
- Catheter ablation eliminates certain rhythm problems causing palpitations. For conditions like supraventricular tachycardia or frequent premature beats from a single source, ablation offers potential cure with high success rates.
- Cognitive behavioral therapy helps people whose palpitations are primarily anxiety-driven or who’ve developed health anxiety about their heartbeat. Learning to reduce hypervigilance about your heart rhythm can significantly improve quality of life.
What Happens If Left Untreated
Consequences of untreated palpitations depend entirely on the underlying cause.
- For benign palpitations from premature beats or anxiety-triggered sinus tachycardia, nothing harmful happens medically if left untreated. Your heart isn’t damaged by feeling palpitations. However, quality of life can suffer significantly.
- Anxiety about palpitations often becomes the main problem. Constant worry about your heart, hypervigilance about every heartbeat, and fear that something is seriously wrong create significant distress. This health anxiety can be more disabling than the palpitations themselves.
- Activity restriction from fear is common. Some people avoid exercise, caffeine, or situations where they’ve experienced palpitations, limiting their lives unnecessarily. This self-imposed restriction reduces quality of life without medical benefit if palpitations are benign.
- Sleep disruption occurs when palpitations are most noticeable at night or when anxiety about them prevents restful sleep.
- If palpitations result from actual rhythm abnormalities that go undiagnosed, consequences vary. Undiagnosed atrial fibrillation increases stroke risk. Frequent premature ventricular contractions can rarely weaken the heart over time if extremely numerous. Unrecognized supraventricular tachycardia continues causing uncomfortable episodes.
- Depression and anxiety disorders can develop or worsen when palpitations create constant fear about your health.
What to Watch For
Most palpitations don’t require emergency care. However, certain situations warrant immediate medical attention.
- Seek emergency care if palpitations are accompanied by severe chest pain, particularly if pain is crushing, radiates to your arm or jaw, or comes with sweating and nausea. These symptoms might indicate a heart attack.
- Call emergency services if you faint or nearly faint with palpitations. Brief lightheadedness is common and not concerning, but actual loss of consciousness needs urgent evaluation.
- Head to the emergency room if palpitations are sustained and rapid (typically you can count rates over 150 beats per minute) and accompanied by severe shortness of breath or extreme dizziness.
- Contact your doctor promptly for palpitations that are new and different from anything you’ve experienced before. First-time significant palpitations warrant evaluation even if they resolve.
- Report to your doctor if palpitation patterns change significantly. If you typically have brief occasional palpitations but suddenly experience sustained episodes, this change needs assessment.
- Seek medical evaluation if palpitations occur during or immediately after exercise, particularly if accompanied by chest pain or extreme fatigue. Exercise-related symptoms can indicate underlying heart disease.
- If you have known heart disease and develop new palpitations, contact your cardiologist. In people with structural heart problems, new rhythm disturbances need prompt evaluation.
- Report palpitations that interfere significantly with daily life, work, or sleep, even if you don’t think they’re dangerous. Quality of life matters, and treatment options exist.
Potential Risks and Complications
For most people, palpitations themselves pose no direct health risks.
- The primary risk is anxiety and reduced quality of life from constant worry about your heart. This psychological impact can be more significant than any physical effects.
- Injury from fainting during palpitations is possible, though uncommon. Falls can cause head trauma or fractures.
- Very frequent palpitations from premature ventricular contractions, typically more than 10,000-15,000 daily sustained over months to years, can rarely weaken heart function. This is uncommon but represents one situation where treating otherwise benign extra beats becomes important.
- Undiagnosed rhythm abnormalities carry specific risks. Unrecognized atrial fibrillation increases stroke risk significantly. Dangerous ventricular rhythms can cause sudden cardiac death if not identified and treated.
- Medication side effects occur if you’re prescribed drugs to control palpitations. Beta-blockers can cause fatigue and exercise intolerance. Antiarrhythmic medications have more serious potential side effects.
- Sleep deprivation from palpitations disrupting sleep affects overall health and quality of life.
- Social isolation can develop if fear of experiencing palpitations in public causes you to avoid social situations.
Diet and Exercise
Lifestyle choices significantly influence palpitation frequency for many people.
- Identify your triggers through careful attention and diary-keeping. Note what you ate, drank, did, or experienced before palpitations. Patterns often emerge—perhaps coffee triggers your symptoms, or they occur when you’re sleep-deprived.
- Reduce or eliminate caffeine if it triggers your palpitations. This doesn’t mean everyone needs to avoid caffeine, but if you notice a connection, limiting intake helps. Remember caffeine is found in coffee, tea, energy drinks, sodas, chocolate, and some medications and supplements.
- Avoid energy drinks, which combine very high caffeine levels with other stimulants and commonly provoke palpitations.
- Limit alcohol if it triggers your symptoms. Some people are particularly sensitive to alcohol’s effects on heart rhythm.
- Stay well-hydrated throughout the day. Dehydration is a common, easily correctable cause of increased palpitations.
- Eat regular balanced meals to maintain stable blood sugar. Skipping meals or extreme dieting can cause blood sugar drops that trigger palpitations.
- Ensure adequate potassium and magnesium intake through diet. Bananas, oranges, potatoes, spinach, nuts, seeds, and whole grains are good sources. However, don’t take supplements without discussing with your doctor, as too much can be harmful.
- Exercise regularly with moderate activity. Physical fitness often reduces palpitation frequency. However, if vigorous exercise triggers your symptoms, discuss appropriate activity levels with your doctor.
- Get adequate sleep consistently. Sleep deprivation increases palpitations in many people. Aim for 7-9 hours nightly with consistent sleep and wake times.
- Manage stress through techniques that work for you—regular exercise, meditation, yoga, deep breathing, counseling, or other methods. Stress is a very common palpitation trigger.
- Avoid recreational drugs, all of which can cause dangerous heart rhythm problems.
Prevention
Since palpitations often result from normal heart rhythm variations or benign extra beats, complete prevention isn’t possible or necessary. However, you can reduce frequency.
- Know and avoid your personal triggers once you’ve identified them through careful attention.
- Maintain good overall cardiovascular health. Control blood pressure, manage weight, treat underlying conditions, and stay physically active.
- Don’t obsessively check your pulse or monitor your heartbeat constantly. Hypervigilance increases anxiety, which can trigger more palpitations. Once you’ve been evaluated and reassured your heart is healthy, try to pay less attention to your heartbeat.
- Practice stress management regularly, not just when you’re overwhelmed. Building stress resilience reduces overall anxiety levels.
- Limit stimulants including caffeine, nicotine, and medications with stimulant properties unless your doctor specifically recommends them.
- Maintain consistent sleep schedules and prioritize good sleep hygiene.
- Stay physically active. Regular moderate exercise improves heart health and often reduces palpitation frequency over time.
- Address anxiety or depression if present. Mental health significantly affects palpitation perception and frequency.
Key Points
- Palpitations are extremely common and usually benign. Nearly everyone experiences them at some point, and they rarely indicate serious heart problems in people without known heart disease.
- The sensation of palpitations doesn’t reliably indicate what’s actually happening with your heart rhythm. You need monitoring during symptoms to know whether you have normal rhythm, harmless extra beats, or actual arrhythmias.
- If you’ve been evaluated and told your heart structure is normal and palpitations are benign, trust that assessment. Anxiety about palpitations often causes more problems than the palpitations themselves.
- Occasional extra beats are completely normal. You have thousands daily without noticing most of them. Simply becoming aware of normal heart function doesn’t mean something is wrong.
- The pattern of palpitations provides clues about their cause. Sudden onset and offset suggest certain rhythm problems. Gradual changes suggest sinus tachycardia or anxiety. Connection to specific triggers points toward those triggers as causes.
- Palpitations that occur only during exercise or are accompanied by other concerning symptoms like chest pain, fainting, or severe shortness of breath warrant prompt evaluation. These patterns are more concerning than isolated palpitations at rest.
- Lifestyle modifications including reducing caffeine, limiting alcohol, managing stress, staying hydrated, and getting adequate sleep help many people reduce palpitations significantly.
- Most people with palpitations don’t need medications or procedures. Simple reassurance and lifestyle adjustments are often sufficient once serious causes have been ruled out.
- If palpitations significantly affect your quality of life, discuss treatment options with your doctor even if they’re not medically dangerous. Quality of life matters, and effective treatments exist for many causes of palpitations.
- Work with your doctor to find the right balance between appropriate evaluation and unnecessary worry. Initial assessment to rule out serious causes is reasonable. Once you know your heart is healthy, try to accept occasional palpitations as a normal variation rather than constantly seeking reassurance through repeated testing. This approach reduces anxiety and often, paradoxically, reduces the palpitations themselves.
You may also like to read these:
Reference: Palpitation