Cholesterol is a fat-like substance (lipid) found in the blood and in every cell of the body. It is essential for normal bodily functions, including hormone production, vitamin D synthesis, and cell membrane structure. However, when cholesterol levels are imbalanced, particularly when harmful forms are elevated, cholesterol becomes a major driver of cardiovascular disease.
High cholesterol itself does not cause symptoms, but over time it significantly increases the risk of atherosclerosis, heart attack, and stroke. Understanding cholesterol types, causes, and treatment options is key to long-term cardiovascular health.
- What Cholesterol Does in the Body
- Types of Cholesterol (Lipid Profile Explained)
- What Is Considered Normal or High?
- Causes of High Cholesterol
- Symptoms of High Cholesterol
- How Cholesterol Is Diagnosed
- Treatment Options for High Cholesterol
- Monitoring and Long-Term Management
- Cholesterol and Cardiovascular Disease
- In Summary
What Cholesterol Does in the Body
Cholesterol is transported through the bloodstream attached to proteins, forming particles called lipoproteins. These particles differ in structure and function, which determines whether cholesterol is protective or harmful.
The body produces most of its cholesterol in the liver, while a smaller portion comes from dietary sources. Problems arise when cholesterol production, clearance, and intake are out of balance.
Types of Cholesterol (Lipid Profile Explained)
A standard blood test called a lipid profile measures different cholesterol components.
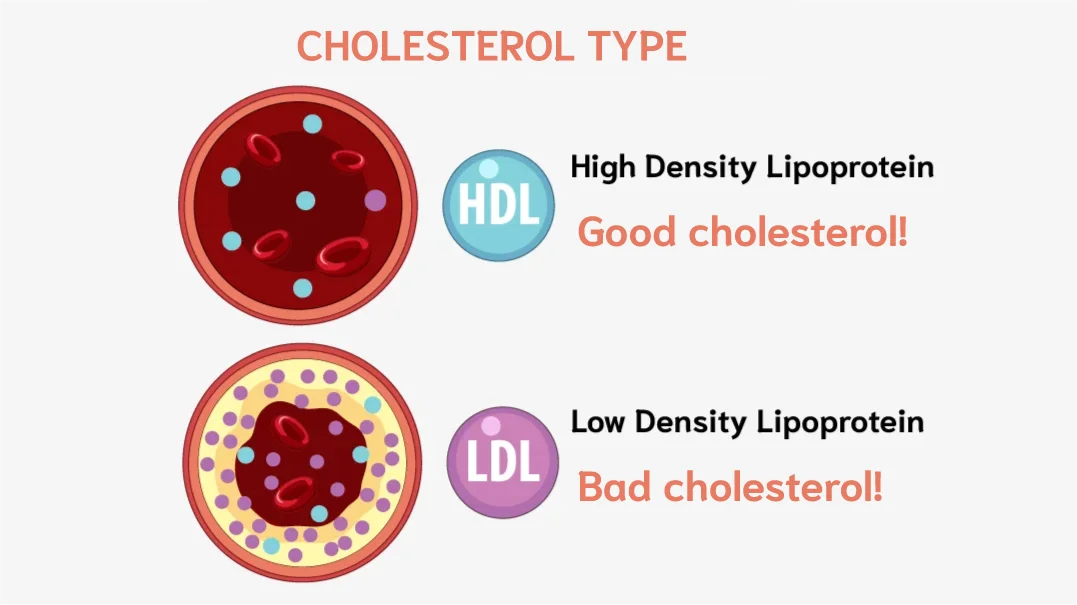
LDL Cholesterol (“Bad” Cholesterol)
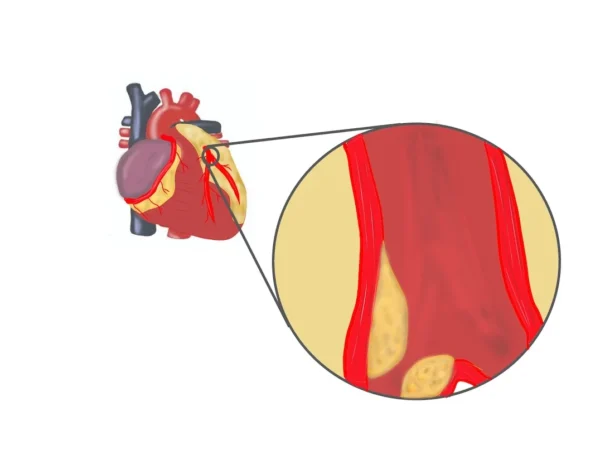
Low-density lipoprotein (LDL) cholesterol carries cholesterol from the liver to tissues. When LDL levels are high, excess cholesterol can deposit in artery walls and contribute to plaque formation.
Elevated LDL cholesterol is the primary target of cholesterol-lowering treatment, as it is strongly linked to cardiovascular events.
HDL Cholesterol (“Good” Cholesterol)
High-density lipoprotein (HDL) cholesterol helps remove excess cholesterol from the bloodstream and transport it back to the liver for elimination.
Higher HDL levels are generally associated with lower cardiovascular risk, although raising HDL alone does not necessarily reduce risk without lowering LDL.
Triglycerides
Triglycerides are another type of blood fat that store excess energy. Elevated triglyceride levels often accompany low HDL and high LDL and are associated with increased cardiovascular risk, particularly when very high.
Total Cholesterol
Total cholesterol represents the combined amount of LDL, HDL, and other lipid particles. While useful for screening, individual components—especially LDL—are more important for risk assessment.
What Is Considered Normal or High?
Cholesterol levels are interpreted based on individual cardiovascular risk, but general reference ranges help guide evaluation and treatment decisions.
LDL cholesterol is the primary target of treatment. For most people, LDL cholesterol is considered optimal when it is below 100 mg/dL. In individuals at very high cardiovascular risk—such as those with known heart disease, prior heart attack, or stroke—treatment often aims to lower LDL cholesterol to around 70 mg/dL or lower.
HDL cholesterol is considered protective. In men, HDL cholesterol is generally considered desirable when it is 40 mg/dL or higher, while in women, levels are considered favorable when they are 50 mg/dL or higher.
Triglyceride levels are considered normal when they are below 150 mg/dL. Higher levels may increase cardiovascular risk, particularly when combined with other lipid abnormalities.
Total cholesterol is often used as a screening measure. Levels are generally considered desirable when total cholesterol is below 200 mg/dL, although individual components—especially LDL cholesterol—are more important for risk assessment.
Ultimately, cholesterol targets are individualized and based on overall cardiovascular risk, including age, blood pressure, diabetes status, smoking history, and the presence of established cardiovascular disease.
Causes of High Cholesterol
High cholesterol usually develops due to a combination of genetic and lifestyle factors.
Genetic Factors
Some individuals inherit conditions that impair cholesterol clearance, leading to very high LDL levels from a young age. These patients often require early and aggressive treatment.
Lifestyle and Metabolic Factors
Diet high in saturated fats, physical inactivity, excess body weight, smoking, diabetes, and metabolic syndrome all contribute to abnormal cholesterol levels.
Aging also affects cholesterol metabolism, increasing cardiovascular risk over time.
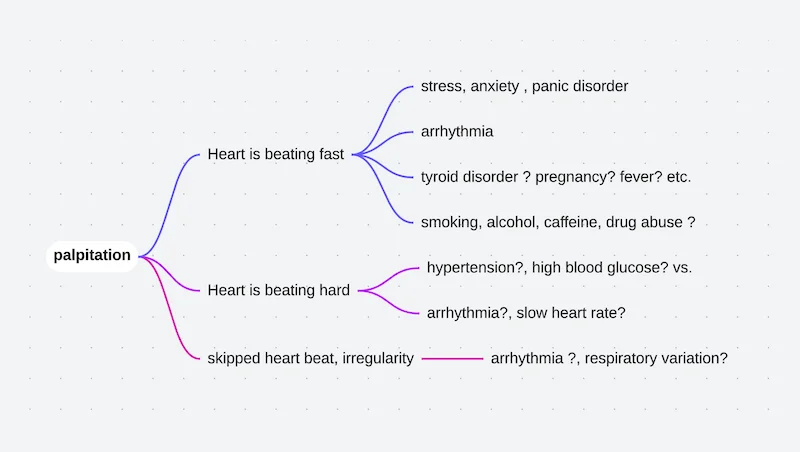
Symptoms of High Cholesterol
High cholesterol does not cause direct, immediate symptoms. Most people feel completely well for years, even when cholesterol levels are significantly elevated. For this reason, high cholesterol is often described as a silent condition.
Symptoms usually appear only after cholesterol has caused damage to blood vessels and led to atherosclerosis or organ-related complications.
Depending on which arteries are affected, symptoms may include:
Heart (coronary arteries):
- Chest pain or pressure with exertion, shortness of breath, fatigue, or—in advanced cases—heart attack
Brain (carotid or cerebral arteries):
- Sudden weakness, speech difficulty, vision problems, dizziness, or stroke
Legs (peripheral arteries):
- Leg pain or cramping during walking that improves with rest, cold feet, slow-healing wounds
Because these symptoms reflect established vascular disease, the goal of cholesterol management is to prevent these complications before they occur. This makes regular screening critically important, even in people who feel healthy.
How Cholesterol Is Diagnosed
Diagnosis is made through a fasting or non-fasting blood lipid panel. Results are interpreted alongside other risk factors such as age, blood pressure, smoking status, diabetes, and family history.
Cholesterol levels are used to estimate long-term cardiovascular risk and guide treatment decisions.
Treatment Options for High Cholesterol
Treatment of high cholesterol focuses on lowering harmful cholesterol levels, stabilizing arterial plaques, and reducing the long-term risk of heart attack, stroke, and other vascular diseases. Management is individualized and often long-term.
Lifestyle Modification
Lifestyle changes are the foundation of cholesterol management for everyone, regardless of whether medication is needed.
Heart-healthy nutrition plays a central role. This includes reducing saturated and trans fats, limiting processed and fried foods, and emphasizing vegetables, fruits, whole grains, legumes, fish, and healthy fats such as olive oil. These changes help lower LDL (“bad”) cholesterol and improve overall vascular health.
Regular physical activity improves cholesterol balance by lowering LDL cholesterol and triglycerides while supporting healthy HDL (“good”) cholesterol levels. Even moderate, consistent exercise has meaningful benefits.
Weight control is particularly important, as excess body weight worsens lipid abnormalities and insulin resistance.
Smoking cessation is critical, as smoking accelerates atherosclerosis regardless of cholesterol level.
Alcohol moderation is advised, as excess intake can raise triglyceride levels.
For individuals with mildly elevated cholesterol and low overall cardiovascular risk, lifestyle changes alone may be sufficient. In higher-risk patients, lifestyle measures enhance—but do not replace—medication therapy.
Cholesterol-Lowering Medications
Medications are recommended when lifestyle measures are insufficient or when a person’s cardiovascular risk is high, even if cholesterol elevation appears modest.
The most commonly used medications are statins, which reduce cholesterol production in the liver and increase removal of LDL cholesterol from the bloodstream. Statins have strong evidence for reducing heart attacks, strokes, and cardiovascular death.
Other oral medications may be added when additional LDL lowering is needed or when statins alone are not tolerated. These drugs work by reducing cholesterol absorption from the intestine or enhancing cholesterol clearance.
Many patients require combination therapy to reach individualized cholesterol targets, especially those with known cardiovascular disease, diabetes, or multiple risk factors.
Advanced and Targeted Therapies
In people with very high cholesterol, established cardiovascular disease, or inherited lipid disorders, standard therapy may not be sufficient.
In these cases, newer injectable or advanced oral therapies can be used to achieve deeper and more consistent LDL cholesterol reduction. These treatments work by enhancing the liver’s ability to clear LDL cholesterol from the blood.
Such therapies are typically reserved for:
- Patients with persistent high LDL cholesterol despite optimal treatment
- Individuals with familial hypercholesterolemia
- Patients at very high cardiovascular risk
Treatment choice is guided by risk level, response to prior therapy, and long-term benefit.
Monitoring and Long-Term Management
Cholesterol management is usually lifelong. Regular follow-up blood tests help assess treatment response and ensure targets are maintained.
Lowering cholesterol does not eliminate plaque immediately, but it stabilizes plaques and reduces the risk of rupture, which is the main cause of heart attacks.
Cholesterol and Cardiovascular Disease
High cholesterol is a major contributor to atherosclerosis, coronary artery disease, stroke, and peripheral artery disease. Reducing LDL cholesterol is one of the most effective strategies for preventing cardiovascular events.
In Summary
Cholesterol is essential for normal body function but becomes harmful when levels—especially LDL cholesterol—are elevated. Because high cholesterol causes no symptoms, regular screening is critical. Management combines lifestyle changes with medication when needed, focusing on long-term risk reduction rather than short-term numbers. With appropriate treatment, cholesterol-related cardiovascular risk can be dramatically reduced.
You may also like to read these:
Reference: Cholesterol