Pulmonary embolism (PE) happens when a blood clot—usually from the veins in your legs or pelvis—travels through the bloodstream and suddenly lodges in an artery of your lungs. This blocks blood flow, reduces oxygen levels, strains your heart, and can become life-threatening within minutes if the clot is large. Some people experience sudden shortness of breath or chest pain, while others may have subtle symptoms for days. Early recognition and treatment with blood thinners or clot-removal procedures dramatically improve outcomes. Because PE can recur, long-term prevention and careful follow-up are essential.
Overview
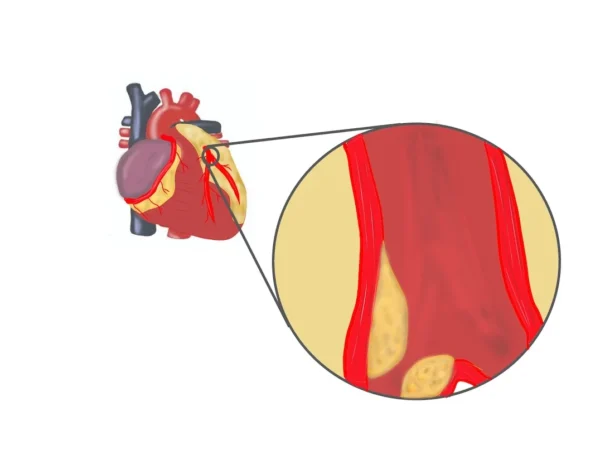
Pulmonary embolism is a blockage of a pulmonary artery in the lungs caused by a blood clot. Nearly all clots originate as deep vein thrombosis (DVT) in the legs or pelvis. When the clot breaks free and travels to the lungs, it becomes a pulmonary embolism.
The severity depends on the clot’s size and location. A small clot may cause mild symptoms, while a large or multiple clots can block major arteries, sharply reducing oxygen supply and potentially causing sudden death. Your right heart chamber must work harder to push blood past the blockage, which can lead to right-sided heart failure.
PE is common and often underdiagnosed. It requires rapid medical evaluation because early treatment significantly reduces the risk of death and long-term complications.
Causes
Pulmonary embolism occurs when a blood clot forms in a vein—most often a deep vein in the leg—and travels to the lungs. This process is called venous thromboembolism (VTE).
Several conditions increase the chance of clot formation:
- A major risk is prolonged immobility, such as long flights, long car rides, or being bedridden after surgery or illness. When leg muscles don’t move, blood flow slows and clots can form.
- Surgery—especially orthopedic, pelvic, or cancer surgery—greatly increases risk because of inflammation, injury to blood vessels, and immobility.
- Pregnancy and the postpartum period increase clotting tendency. Hormonal birth control and hormone replacement therapy can also increase risk.
- Cancer and chemotherapy make blood more prone to clotting.
- Inherited clotting disorders, like factor V Leiden or prothrombin gene mutation, make clots more likely even at young ages.
- Trauma, fractures, or severe infections raise the risk. Smoking, obesity, dehydration, and certain chronic illnesses also contribute.
Sometimes PE happens without an identifiable trigger, especially in people with genetic or subtle clotting abnormalities.
Symptoms
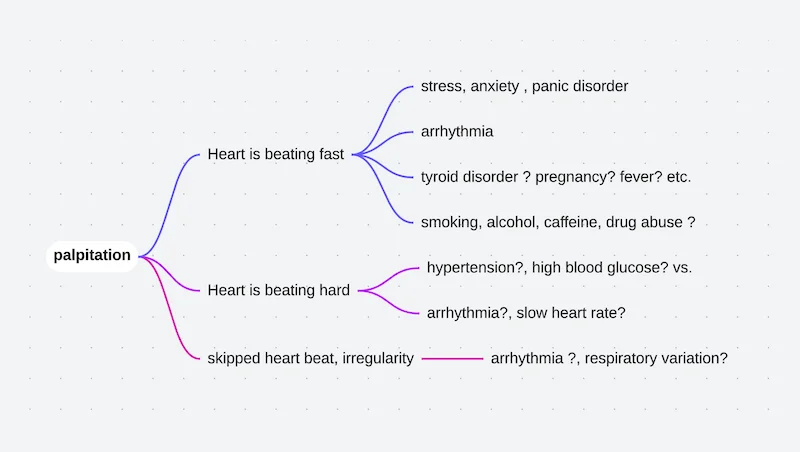
Pulmonary embolism has a wide range of symptoms, depending on clot size and how much of the lung is affected.
- The most common symptom is sudden shortness of breath. You may feel like you can’t take a deep breath or like you’re breathing faster than usual.
- Sharp or stabbing chest pain that worsens with deep breaths or coughing is common. This pain often mimics heart-related chest pain.
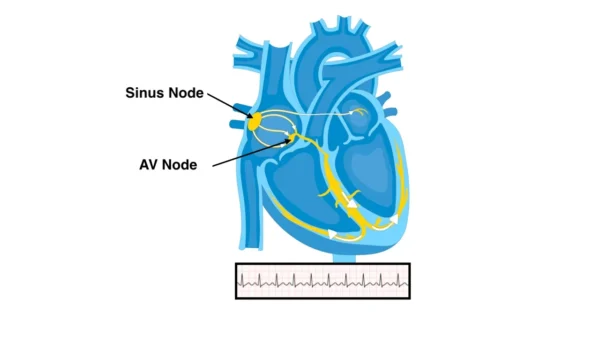
- A rapid heartbeat, lightheadedness, or fainting can occur if the clot is large.
- A persistent cough may appear, sometimes producing blood-streaked mucus.
- Low-grade fever, sweating, anxiety, or a sense of doom can accompany the event.
- Many people also have signs of deep vein thrombosis—leg swelling, redness, warmth, or tenderness—especially in one leg.
- Symptoms vary widely; some people have mild discomfort, while others collapse suddenly if the clot is massive.
Diagnosis
Diagnosing pulmonary embolism requires a combination of clinical assessment, imaging, and blood tests because symptoms can mimic many other conditions.
- The first step is assessing your symptoms, vital signs, and risk factors. Doctors often use clinical scoring systems to estimate the likelihood of PE.
- A CT pulmonary angiography (CTPA) is the most common and accurate test. It shows the blood vessels in the lungs and identifies clots.
- If CT cannot be used—such as in pregnancy or kidney problems—a ventilation/perfusion (V/Q) scan evaluates airflow and blood flow mismatches in the lung.
- A D-dimer blood test helps rule out PE in low-risk patients; a normal result makes PE unlikely.
- Ultrasound of the legs can detect DVT, especially when imaging the chest is not possible.
- An echocardiogram may show strain on the right side of the heart in severe cases.
Diagnosis is based on combining clinical suspicion with imaging results.
Treatment
Treatment depends on the severity of the clot, your symptoms, and your risk of complications. The primary goal is to stop the clot from growing and prevent new clots.
- Most patients start anticoagulant (blood thinner) medications, such as heparin or direct oral anticoagulants. These don’t dissolve the clot but prevent growth and allow the body to absorb it over time.
- People with large or life-threatening clots may need thrombolytic therapy, which uses powerful medications to dissolve the clot quickly. This is reserved for severe cases due to bleeding risks.
- Catheter-based treatments may be used to physically remove or break up the clot, especially when thrombolytics are too risky.
- In rare cases, surgery is required to remove massive clots.
- If anticoagulants cannot be used, an inferior vena cava (IVC) filter may be placed to catch clots before they reach the lungs.
- Long-term treatment typically continues for at least three to six months, and longer if the risk of recurrence is high.
What Happens If Left Untreated
- Untreated pulmonary embolism can be rapidly fatal. Large clots can cause sudden collapse, severe low oxygen levels, and cardiac arrest.
- Even smaller untreated clots cause long-term strain on the right side of the heart, potentially leading to chronic thromboembolic pulmonary hypertension (CTEPH), a serious condition that causes persistent breathlessness and reduced exercise capacity.
- Fragments of the clot can continue blocking smaller vessels, gradually worsening lung function.
- Because untreated PE can progress quickly, immediate evaluation is essential for anyone with sudden unexplained shortness of breath or chest pain.
What to Watch For
- Sudden or unexplained shortness of breath should always be taken seriously, especially if you recently had surgery, a long flight, a leg injury, or a period of immobility.
- Chest pain that worsens with breathing, rapid heartbeat, fainting spells, or coughing up blood are red-flag symptoms.
- New swelling, redness, or pain in one leg may signal a deep vein thrombosis and should be evaluated promptly to prevent PE.
- People with cancer, clotting disorders, or a history of PE should be alert to early symptoms and seek care immediately.
Living with Pulmonary Embolism
Recovery from PE involves medication adherence, lifestyle adjustments, and monitoring for recurrence.
- Taking anticoagulants exactly as prescribed is crucial; missing doses increases the risk of another clot. Regular blood tests may be needed depending on the medication.
- Staying active, walking regularly, maintaining a healthy weight, and avoiding dehydration reduce risk.
- If you had a provoked PE—such as after surgery or immobility—your long-term risk may be lower. If you had an unprovoked or recurrent PE, long-term or lifelong anticoagulation may be recommended.
- People with ongoing shortness of breath after treatment may need follow-up testing to look for chronic complications.
- Managing other medical issues—such as cancer, hormonal therapy, or clotting disorders—is essential for preventing recurrence.
Key Points
- Pulmonary embolism is a blockage of an artery in the lungs, usually caused by a blood clot that traveled from the legs.
- Symptoms range from mild shortness of breath to sudden collapse. Early recognition saves lives.
- Diagnosis relies on CT pulmonary angiography, D-dimer testing, and ultrasound for DVT.
- Treatment includes blood thinners, clot-dissolving medications, or procedures to remove the clot.
- Untreated PE can be fatal or lead to long-term lung and heart complications.
- Prevention and long-term management depend on reducing clotting risk, taking medications correctly, and addressing underlying factors.
Reference: Pulmonary Embolism