Tachycardia is a condition in which the heart beats faster than normal at rest. For most adults, a resting heart rate above 100 beats per minute is considered tachycardia. While a fast heartbeat can be a normal response to exercise, stress, or excitement, tachycardia refers to situations where the heart rate is inappropriately fast or occurs without a clear reason.
Not all tachycardia is dangerous. Some forms are temporary and harmless, while others may signal an underlying arrhythmia that requires medical attention. Understanding the difference is key to knowing when to be reassured and when to seek care.
- How Heart Rate Normally Works
- Symptoms of Tachycardia
- Why Tachycardia Occurs
- Sinus Tachycardia: When a Fast Heart Rate Is Normal
- Different Types of Tachycardia
- How Tachycardia Is Diagnosed
- When Tachycardia Becomes a Problem
- Treatment Approach for Tachycardia
- Preventing Recurrence
- Living With Tachycardia
- In Summary
How Heart Rate Normally Works
The heart is designed to adjust its speed based on the body’s needs. During physical activity or emotional stress, the heart beats faster to deliver more oxygen-rich blood. Once the trigger passes, the heart rate slows back down.
Tachycardia becomes a concern when the heart continues to beat too fast at rest, starts suddenly without an obvious trigger, or causes symptoms. In these situations, the fast rate is usually driven by abnormal electrical activity rather than normal physiological demand.
Symptoms of Tachycardia
The way tachycardia feels can differ widely. Some people are very aware of every fast beat, while others notice only subtle changes.
Before listing symptoms, it is important to note that the presence or absence of symptoms does not always reflect severity. Some serious rhythm disorders may cause little discomfort, while benign ones can feel dramatic.
Common symptoms include:
- A sensation of a racing or pounding heartbeat
- Palpitations felt in the chest or neck
- Shortness of breath
- Lightheadedness or dizziness
- Chest discomfort
- Fatigue or weakness
In more pronounced cases, tachycardia may lead to near-fainting or fainting, especially if blood flow to the brain is temporarily reduced.
Why Tachycardia Occurs
Tachycardia can arise for many reasons, and not all of them originate in the heart itself. Sometimes the heart is responding appropriately to another condition in the body.
Common causes include:
- Physical exertion, anxiety, or emotional stress
- Fever, dehydration, or infection
- Anemia or low blood oxygen levels
- Thyroid disorders
- Caffeine, nicotine, or stimulant use
- Certain medications
In other cases, tachycardia is caused by a primary heart rhythm disorder. These conditions involve abnormal electrical pathways or signals within the heart and may lead to recurrent or persistent episodes.
Sinus Tachycardia: When a Fast Heart Rate Is Normal
Not every fast heartbeat is caused by an abnormal rhythm. In many situations, the heart speeds up for appropriate and healthy reasons. This is known as sinus tachycardia.
In sinus tachycardia, the heart rhythm itself remains normal. The electrical signals follow the usual pathway, but they occur more frequently. This often happens during physical activity, emotional stress, fever, dehydration, pain, or in response to conditions such as anemia or thyroid disorders.
The key difference is that sinus tachycardia is a response, not a malfunction. Once the underlying trigger is addressed—such as treating an infection, correcting dehydration, or reducing stress—the heart rate usually returns to normal without the need for rhythm-specific treatment.
Distinguishing sinus tachycardia from abnormal rhythm disorders is essential, as the approach focuses on identifying and correcting the cause rather than treating the heart’s electrical system itself.
In some individuals, however, the heart rate remains persistently elevated even at rest and without an identifiable trigger. This condition is known as Inappropriate Sinus Tachycardia. Although the heart rhythm is technically normal, the abnormally high rate can cause significant symptoms such as palpitations, fatigue, and exercise intolerance, and may require targeted medical management rather than simple reassurance.
Different Types of Tachycardia
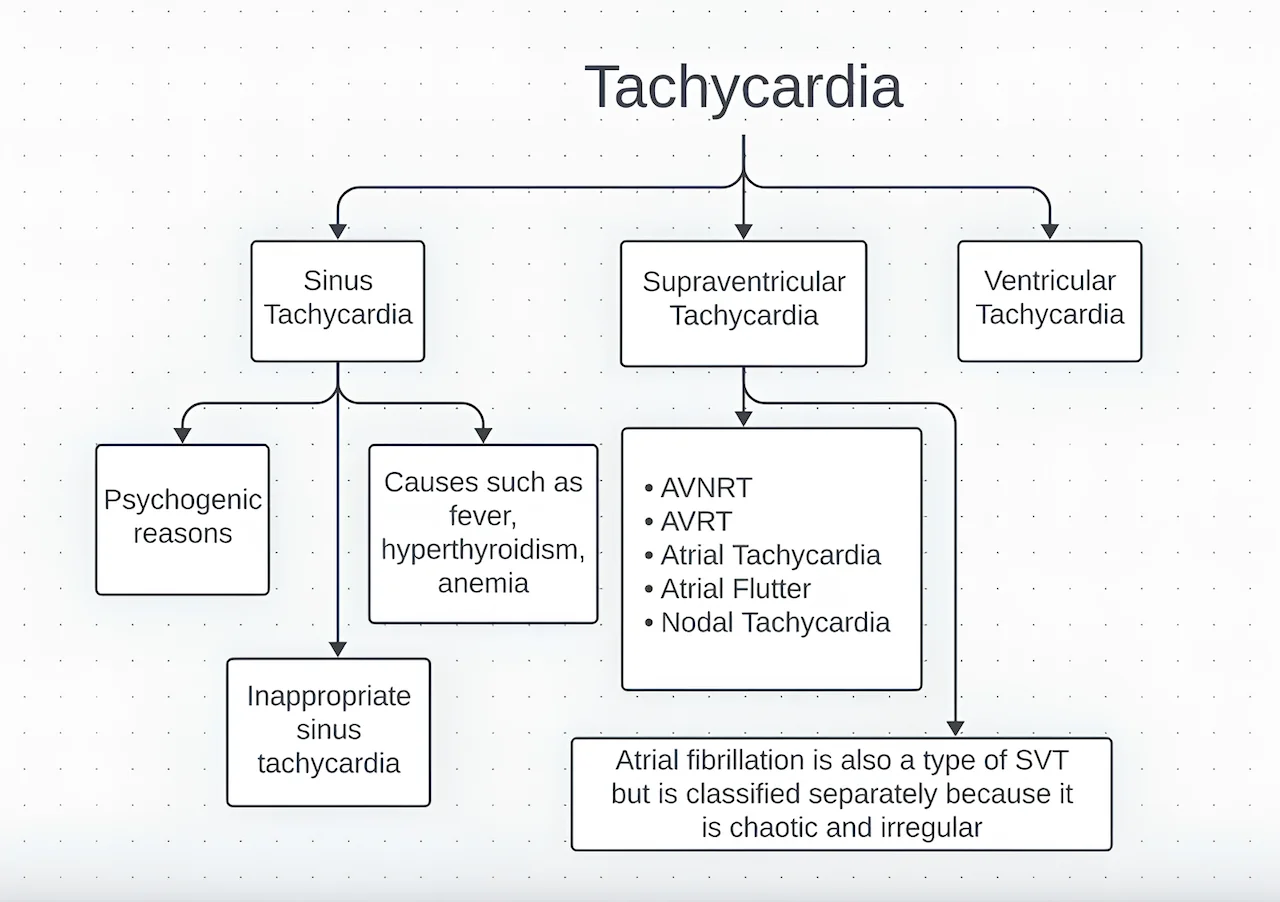
Not all fast heart rhythms are the same. Tachycardia is a broad term that includes several distinct rhythm patterns, depending on where in the heart the fast rhythm begins and how the electrical signals behave.
Some tachycardias originate in the upper chambers of the heart. These are known as Supraventricular Tachycardia (SVT) and typically start and stop suddenly. SVT episodes are often fast but regular and are commonly seen in people with otherwise healthy hearts. Although symptoms can be intense, these rhythms are usually not life-threatening and are often highly treatable.
Another common form of tachycardia is Atrial Fibrillation, in which the heart beats fast and irregularly due to chaotic electrical activity in the atria. Unlike SVT, this rhythm does not usually start and stop abruptly and carries an increased risk of stroke, making long-term management particularly important.
Some fast rhythms begin in the lower chambers of the heart. These are referred to as Ventricular Tachycardia and are generally more serious. Because the ventricles are responsible for pumping blood to the body, fast rhythms arising from this area can significantly impair circulation and may be life-threatening, especially in people with underlying heart disease.
There is also a form of tachycardia that reflects a normal rhythm behaving faster than usual rather than an abnormal circuit. This is called Sinus Tachycardia. It often occurs in response to exercise, stress, fever, dehydration, or other medical conditions and usually resolves once the underlying cause is addressed.
Understanding which type of tachycardia is present is essential because treatment, risk, and long-term outlook differ greatly between these rhythm patterns. Identifying the exact mechanism allows care to be tailored to the individual rather than treating all fast heart rates as the same condition.
How Tachycardia Is Diagnosed
Diagnosis starts with documenting the heart rhythm. An electrocardiogram records the heart’s electrical activity and can often identify the type of tachycardia when it is present.
Because some episodes are brief or infrequent, longer-term monitoring may be needed. Additional tests may be used to evaluate heart structure, blood flow, and conditions that could be triggering the fast rhythm.
The goal of diagnostic testing is not only to confirm tachycardia, but also to determine its cause and potential impact on overall heart health.
When Tachycardia Becomes a Problem
Occasional fast heartbeats are common and often harmless. Tachycardia becomes concerning when it occurs frequently, lasts for long periods, causes significant symptoms, or is associated with underlying heart disease.
Sustained or poorly controlled tachycardia can place extra strain on the heart. Over time, this may weaken the heart muscle or worsen existing heart conditions. For this reason, persistent tachycardia should not be ignored.
Treatment Approach for Tachycardia
Treatment depends entirely on the underlying cause. In some cases, no specific treatment is needed beyond reassurance and trigger avoidance. In others, addressing contributing conditions such as dehydration, thyroid imbalance, or anemia resolves the problem.
When tachycardia is caused by a heart rhythm disorder, treatment may include medications to slow the heart rate or stabilize the electrical system. In selected cases, procedures aimed at correcting abnormal electrical pathways may be recommended.
The goal is not simply to slow the heart rate, but to restore a rhythm that allows the heart to function efficiently and safely.
Preventing Recurrence
Many forms of tachycardia can be influenced by lifestyle factors. Staying well hydrated, managing stress, limiting stimulant intake, and treating underlying medical conditions all play an important role in prevention.
For individuals with recurrent episodes, understanding personal triggers and maintaining regular medical follow-up can significantly reduce both frequency and severity.
Living With Tachycardia
Living with tachycardia can be unsettling, especially when episodes are unpredictable. Education is a powerful tool. Knowing what type of tachycardia is present, what triggers it, and how it is managed helps reduce anxiety and improves confidence in daily life.
With appropriate evaluation and individualized care, most people with tachycardia can lead active, unrestricted lives.
In Summary
Tachycardia refers to a faster-than-normal heart rate and can range from a normal physiological response to a sign of an underlying rhythm disorder. Distinguishing between these possibilities is essential. While many cases are benign, persistent or symptomatic tachycardia deserves proper evaluation to ensure long-term heart health and safety.
Reference: Tachycardia