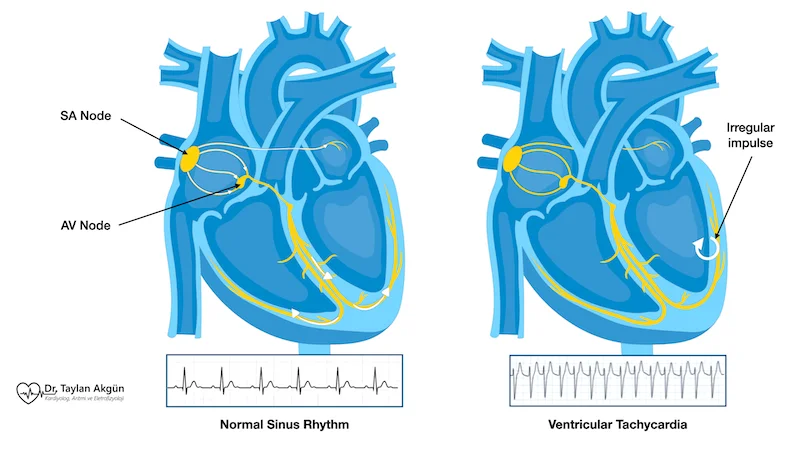
When the lower chambers of your heart suddenly start beating dangerously fast, it creates a condition called ventricular tachycardia. Unlike the more common rapid rhythms originating from your heart’s upper chambers, ventricular tachycardia is always taken seriously because it can quickly deteriorate into life-threatening situations. Your ventricles are responsible for pumping blood throughout your body, and when they beat too rapidly, this critical function becomes severely impaired. Understanding ventricular tachycardia helps you recognize warning signs and appreciate why immediate treatment is essential for this potentially fatal rhythm disorder.
Overview
Ventricular tachycardia, often abbreviated as VT, is a rapid heart rhythm originating in your heart’s lower chambers—the ventricles. The rate is typically 120-250 beats per minute or faster, though what makes VT concerning isn’t just the speed but where it originates and how it affects blood flow.
Your ventricles are the main pumping chambers, responsible for sending blood to your lungs and the rest of your body. When they beat too fast from an abnormal electrical source, they can’t fill properly between beats, dramatically reducing the amount of blood pumped with each contraction. This can cause collapse, loss of consciousness, or progress to ventricular fibrillation—a chaotic rhythm where the heart quivers rather than pumps, causing cardiac arrest.
VT is classified by duration and underlying heart condition. Non-sustained VT lasts less than 30 seconds and stops on its own. Sustained VT continues for 30 seconds or longer, or causes symptoms requiring termination before 30 seconds. Monomorphic VT has a consistent pattern on electrocardiogram, suggesting it originates from a single location. Polymorphic VT has a varying pattern, indicating multiple sources or circuits, and is often more unstable.
The presence or absence of structural heart disease fundamentally affects VT’s significance. VT in people with normal hearts, while still serious, is often less immediately dangerous and more treatable. VT in people with previous heart attacks, heart failure, or cardiomyopathy carries much higher risk because the diseased heart tolerates rapid rates poorly and is more prone to deterioration into cardiac arrest.
Some VT occurs in specific situations. Exercise-induced VT appears during or immediately after physical activity. Torsades de pointes is a specific polymorphic VT related to prolonged electrical recovery time in the heart, often triggered by medications or electrolyte imbalances. Catecholaminergic polymorphic VT is an inherited condition where adrenaline triggers dangerous rhythms.
VT is much less common than rhythms originating in the upper chambers, but its potential severity means it always requires thorough evaluation and usually aggressive treatment.
Causes
VT develops when abnormal electrical activity originates in the ventricles rather than following the normal pathway from your heart’s natural pacemaker.
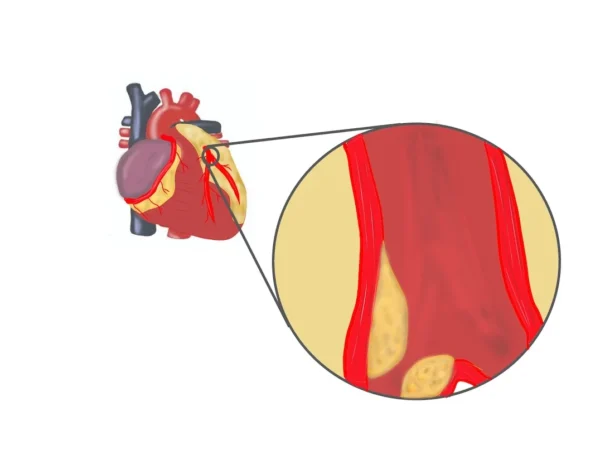
- Previous heart attacks are the most common cause in adults. When heart muscle dies from blocked blood flow, scar tissue forms. These scars create abnormal electrical circuits where signals can circle continuously, triggering VT. The more extensive the heart damage, the higher the VT risk. This is why people who’ve had large heart attacks are at particular risk.
- Cardiomyopathy, or disease of the heart muscle, creates conditions for VT. Dilated cardiomyopathy, where the heart enlarges and weakens, disrupts normal electrical pathways. Hypertrophic cardiomyopathy, where the heart muscle thickens abnormally, creates disorganized tissue prone to dangerous rhythms. Arrhythmogenic right ventricular cardiomyopathy involves replacement of heart muscle with fatty or fibrous tissue, particularly affecting the right ventricle.
- Heart failure from any cause increases VT risk. The stretched, weakened heart muscle becomes electrically unstable.
- Inherited conditions cause VT in people with structurally normal hearts. Long QT syndrome prolongs the heart’s electrical recovery time, creating conditions for torsades de pointes. Brugada syndrome affects sodium channels in heart cells, causing specific VT patterns. Catecholaminergic polymorphic VT is triggered by adrenaline during exercise or stress.
- Electrolyte imbalances severely affect heart rhythm. Low potassium, low magnesium, or abnormal calcium levels can trigger VT. This is why electrolyte monitoring is crucial in hospitalized patients.
- Medications sometimes cause VT, particularly those that prolong electrical recovery time. Some antibiotics, antipsychotics, and even certain heart rhythm medications can paradoxically trigger dangerous rhythms. Drug interactions increase risk.
- Myocarditis, or inflammation of the heart muscle from infection or autoimmune disease, can cause VT during the acute phase.
- Coronary artery disease without previous heart attack can cause VT, particularly during episodes of reduced blood flow to the heart muscle.
- Valvular heart disease, particularly aortic stenosis, sometimes leads to VT as the heart muscle thickens and becomes electrically unstable.
In some cases, VT occurs without identifiable structural heart disease or clear cause. This idiopathic VT, while still serious, often has better prognosis than VT associated with significant heart disease.
Symptoms
VT symptoms vary dramatically based on rate, duration, and underlying heart function. Some people remain conscious and relatively comfortable during VT, while others collapse immediately.
- Palpitations are common if you remain conscious. You feel your heart racing, often with a pounding sensation in your chest. The rapid rate is sustained and regular, different from the irregular pounding of atrial fibrillation.
- Dizziness and lightheadedness occur because your brain isn’t receiving adequate blood flow. The rapid ventricular rate prevents chambers from filling properly, dramatically reducing cardiac output. You might feel like you’re about to faint or lose consciousness.
- Chest pain or pressure develops because the heart muscle isn’t receiving enough oxygen while working so hard. This pain differs from heart attack pain but can be concerning.
- Shortness of breath happens because your lungs aren’t receiving adequate blood flow for oxygenation. You might feel like you can’t catch your breath or need to gasp for air.
- Weakness or fatigue is profound. Your muscles aren’t receiving adequate blood supply, making even standing difficult.
- Loss of consciousness occurs if cardiac output drops critically. Fainting from VT is a medical emergency because it indicates severely inadequate blood flow and high risk of deterioration into cardiac arrest.
- Some people experience sudden collapse without warning, particularly with very rapid VT or polymorphic patterns. One moment you’re conscious, the next you’re on the ground with no memory of what happened.
- Cardiac arrest represents VT’s most dangerous outcome. The rhythm deteriorates into ventricular fibrillation, where the heart quivers ineffectively rather than pumping. Without immediate defibrillation, this is fatal within minutes.
Importantly, brief episodes of non-sustained VT might cause no symptoms at all. These episodes are often discovered incidentally on heart monitors worn for other reasons.
Diagnosis
Diagnosing VT requires capturing the rhythm on monitoring equipment and determining its cause.
- An electrocardiogram during an episode definitively diagnoses VT. The tracing shows characteristic wide, rapid beats originating from the ventricles rather than following normal pathways. The pattern helps distinguish monomorphic from polymorphic VT and provides clues about where the rhythm originates.
- Emergency situations often mean diagnosis occurs simultaneously with treatment. If you collapse or lose consciousness, paramedics or emergency room staff obtain an immediate electrocardiogram while preparing for potential defibrillation.
- Extended monitoring captures intermittent VT. Holter monitors worn for 24-48 hours, event monitors used for weeks or months, or implantable loop recorders placed under chest skin for up to three years can all capture episodes that don’t occur during clinic visits.
- If you have an implantable cardioverter-defibrillator (ICD), it automatically records all VT episodes, storing detailed information about rate, duration, and how the episode terminated. This data is invaluable for understanding your rhythm patterns.
- Blood tests check for underlying causes and contributing factors. Electrolyte panels measure potassium, magnesium, and calcium. Troponin levels detect heart muscle damage. Thyroid function tests identify hormonal imbalances.
- Echocardiography evaluates heart structure and function. This ultrasound shows whether you have previous heart damage, how well your heart pumps, valve function, and other structural abnormalities. The ejection fraction—the percentage of blood pumped with each beat—is particularly important for risk assessment and treatment decisions.
- Cardiac catheterization might be performed to evaluate coronary arteries. If VT results from coronary artery disease, identifying and treating blockages is essential.
- Cardiac MRI provides detailed images of heart muscle, identifying scar tissue from previous heart attacks or areas of abnormal tissue in cardiomyopathy. This information helps plan ablation procedures.
- Electrophysiology studies map your heart’s electrical system in detail. Catheters inserted into your heart record electrical activity and can trigger VT in a controlled environment, allowing precise identification of where the rhythm originates. This is often performed immediately before ablation.
- Genetic testing might be recommended if inherited conditions are suspected, particularly in young people or those with family history of sudden cardiac death.
- Exercise stress testing evaluates whether physical activity triggers VT, important for determining safe activity levels and treatment planning.
Treatment
VT treatment is always urgent and depends on whether you’re stable or in immediate danger.
- Emergency treatment for sustained VT with loss of consciousness or cardiovascular collapse requires immediate defibrillation. Electrical shocks delivered through pads on your chest reset the heart rhythm. If you’ve already progressed to cardiac arrest, CPR is performed until defibrillation is available.
- For conscious patients with stable VT, immediate treatment options include medications given intravenously. Amiodarone, lidocaine, or procainamide can terminate VT episodes. If medications don’t work quickly, synchronized cardioversion under sedation delivers electrical shocks to restore normal rhythm.
- Treating underlying causes is crucial. If electrolyte imbalances triggered VT, correcting them is essential. If medications caused the problem, stopping them and never using them again is critical. If active heart attack is causing VT, emergency procedures to restore blood flow are necessary.
- Long-term prevention focuses on reducing VT recurrence risk. Implantable cardioverter-defibrillators (ICDs) are the cornerstone of treatment for people at high risk of life-threatening VT. These devices continuously monitor heart rhythm and automatically deliver shocks to terminate dangerous rhythms. ICDs don’t prevent VT but ensure it doesn’t cause death.
- Antiarrhythmic medications help reduce VT frequency. Amiodarone, sotalol, mexiletine, and other drugs suppress abnormal electrical activity. These medications often have significant side effects and require regular monitoring.
- Beta-blockers reduce VT risk, particularly in people with previous heart attacks or heart failure. By blocking adrenaline effects, they stabilize heart rhythm and improve survival.
- Catheter ablation destroys tissue causing VT. For VT with identifiable sources, particularly in people with previous heart attacks where scar tissue creates circuits, ablation can significantly reduce VT burden. Success rates vary based on heart disease extent and VT characteristics. Some people become VT-free after ablation, while others experience reduced frequency, allowing medication dose reduction or decreasing ICD shock frequency.
- Treating underlying heart disease improves VT control. Coronary artery bypass surgery or stenting for blocked arteries, medications optimizing heart failure management, and lifestyle modifications all contribute to reducing VT risk.
- For inherited conditions causing VT, treatment is specialized. Beta-blockers are essential for long QT syndrome and catecholaminergic polymorphic VT. ICDs are often recommended. Avoiding triggers specific to each condition is crucial.
What Happens If Left Untreated
Untreated VT carries extremely high risk, though specific outcomes depend on VT type and underlying heart condition.
- Sustained VT inevitably leads to collapse and loss of consciousness as cardiac output becomes inadequate to maintain brain function. This typically occurs within seconds to minutes of VT onset, depending on rate and heart function.
- Progression to ventricular fibrillation is common with sustained VT. This transition from rapid but organized beating to chaotic quivering means your heart stops effectively pumping. Without immediate defibrillation, ventricular fibrillation is fatal within minutes.
- Sudden cardiac death is the ultimate consequence of untreated sustained VT. Even brief delays in treatment can be fatal, which is why people at risk often receive ICDs for immediate automatic treatment.
- For non-sustained VT that stops on its own, the risk is more nuanced. In people with normal hearts, brief episodes might be relatively benign. In people with significant heart disease, even non-sustained VT indicates high risk for sustained episodes and warrants aggressive treatment.
- Frequent VT episodes, even if non-sustained, can weaken the heart over time. The rapid rates stress already diseased heart muscle, potentially worsening heart failure.
- Sudden death during sleep, exercise, or daily activities represents the tragedy of untreated VT. Many sudden cardiac deaths in people with heart disease result from ventricular arrhythmias that could have been prevented with appropriate treatment.
- Quality of life suffers immensely when living with untreated VT risk. Constant fear of sudden collapse or death affects every aspect of daily life.
What to Watch For
If you have risk factors for VT or known heart disease, certain symptoms require immediate action.
- Call emergency services immediately for sustained rapid heartbeat with severe dizziness, chest pain, or feeling like you might lose consciousness. Don’t attempt to drive yourself to the hospital.
- Any loss of consciousness requires emergency evaluation, particularly if you have heart disease. Fainting could represent VT that spontaneously terminated, but you need immediate assessment.
- If you have an ICD and it delivers a shock, follow your doctor’s instructions. One shock typically means calling your doctor promptly. Multiple shocks indicate electrical storm—a medical emergency requiring immediate hospital evaluation.
- New or worsening palpitations that feel different from what you’ve experienced before warrant prompt medical contact, particularly if they’re sustained, rapid, and regular.
- For people with inherited conditions causing VT, symptoms during exercise or emotional stress need immediate attention. These patterns suggest dangerous rhythms that require treatment adjustment.
- If you’re taking medications for VT and develop new symptoms suggesting side effects—lung problems, liver issues, thyroid changes, or vision problems with amiodarone, for example—contact your doctor promptly.
- Family members should learn CPR if you’re at risk for VT. Immediate bystander CPR dramatically improves survival if VT causes cardiac arrest.
Potential Risks and Complications
VT itself is the complication—a dangerous rhythm that can cause death. However, treatments also carry risks.
- ICD complications include infection at the device site, lead problems where wires connect to your heart, inappropriate shocks when the device misinterprets normal rhythms, and the psychological impact of receiving shocks. Despite these issues, ICDs dramatically improve survival in appropriate patients.
- Antiarrhythmic medication side effects vary by drug. Amiodarone can affect lungs, liver, thyroid, and eyes, requiring regular monitoring. Sotalol can paradoxically cause different dangerous rhythms. All antiarrhythmics can have effects on multiple organ systems.
- Catheter ablation carries risks including bleeding, blood vessel damage, heart perforation, and stroke. For VT ablation in people with significant heart disease, risks are somewhat higher than for ablation of rhythms in normal hearts, but benefits often justify these risks when VT is frequent or medication-resistant.
- The psychological toll of living with VT risk is significant. Anxiety about sudden death, the impact of ICD shocks, and restrictions on activities all affect mental health and quality of life.
Living with VT Risk
If you have VT or are at high risk, certain adjustments help you live as normally as possible while staying safe.
- Follow all medication instructions precisely. Skipping antiarrhythmic drugs or heart failure medications increases VT risk significantly.
- If you have an ICD, understand how it works and what to expect. Most people adapt well to having the device, though receiving shocks can be psychologically challenging. Support groups help many people cope.
- Activity recommendations depend on your specific situation. Some people with well-controlled VT can exercise normally, while others need restrictions. Discuss appropriate activities with your doctor. Generally, avoiding extreme exertion and competitive sports is recommended.
- Driving restrictions often apply after VT episodes or ICD shocks. Regulations vary by location but typically prohibit driving for several months after events. This protects you and others from accidents if VT causes loss of consciousness while driving.
- Emotional stress management is important. Adrenaline can trigger VT, particularly in certain inherited conditions. Stress reduction techniques, adequate sleep, and avoiding excessive stimulants help.
- Avoid medications that prolong electrical recovery time in the heart. Many antibiotics, antihistamines, and psychiatric medications can trigger torsades de pointes. Always inform all doctors about your VT history before starting new medications.
- Stay well-hydrated and maintain proper electrolyte balance, particularly if you take diuretics. Low potassium or magnesium increases VT risk.
- Regular follow-up with a cardiologist specializing in heart rhythm disorders is essential. Treatment often requires adjustments based on how you’re doing and whether VT recurs.
Key Points
- Ventricular tachycardia is always taken seriously because it originates in your heart’s main pumping chambers and can quickly become life-threatening. Unlike upper chamber rhythms that are often benign, VT requires urgent evaluation and aggressive treatment.
- The presence of underlying heart disease dramatically affects VT significance. Previous heart attacks, heart failure, or cardiomyopathy make VT particularly dangerous and more likely to recur.
- ICDs are lifesaving for people at high risk of sustained VT. While the devices don’t prevent VT, they ensure dangerous rhythms don’t cause death by automatically delivering treatment within seconds.
- Brief, non-sustained VT might cause no symptoms but still indicates increased risk requiring evaluation. Just because it stops on its own doesn’t mean it’s harmless.
- Treatment combines multiple approaches. ICDs provide safety, medications reduce VT frequency, ablation can eliminate VT sources, and treating underlying heart disease improves overall control.
- Living with VT or VT risk requires adjustments but doesn’t mean giving up all activities. Many people with appropriate treatment live full, active lives while managing their condition.
- If you have risk factors for VT—previous heart attack, heart failure, cardiomyopathy, or family history of sudden cardiac death—discuss screening and prevention with a cardiologist. Early identification and treatment of high-risk individuals prevents sudden cardiac death.
- Sudden cardiac death in people with heart disease is often caused by ventricular arrhythmias. Appropriate evaluation and treatment of those at risk is the most effective prevention strategy we have against this tragic outcome.
- Work closely with a cardiologist experienced in managing ventricular arrhythmias. These complex conditions require specialized knowledge, and treatment is highly individualized based on your specific heart condition, VT characteristics, symptoms, and overall health. The goal is always maximizing both safety and quality of life.
Reference: Ventricular Tachycardia